Diet and Gastrointestinal Problems - Disorders of the Primary Organs | Nutrition and Diet Therapy: Diet and Gastrointestinal Problems
Chapter: Nutrition and Diet Therapy: Diet and Gastrointestinal Problems
Disorders of the Primary Organs
DISORDERS OF THE PRIMARY
ORGANS
Dyspepsia
Dyspepsia, or indigestion, is a
condition of discomfort in the digestive tractthat can be physical or
psychological in origin. Symptoms include heartburn, bloating, pain and,
sometimes, regurgitation. If the cause is physical, it can be due to overeating
or spicy foods, or it may be a symptom of another problem, such as appendicitis
or a kidney, gallbladder, or colon disease or possibly cancer. If the problem
is organic in origin, treatment of the underlying cause will be the normal
procedure.
Psychological stress
can affect stomach secretions and trigger dyspepsia.
Treatment should
include counseling to help the client:
• Find relief from the underlying stress
• Allow sufficient time to relax and enjoy meals
• Learn to improve eating habits
Esophagitis
Esophagitis is caused by the
irritating effect of acidic gastric reflux on themucosa of the esophagus.
Heartburn, regurgitation, and dysphagia (diffi-culty swallowing) are common
symptoms. Acute esophagitis is caused by ingesting an irritating agent, by
intubation, or by an infection. Chronic, or reflux, esophagitis is caused by
recurrent gastroesophageal
reflux (GER). This can be caused by a hiatal hernia, reduced lower esophageal
sphincter (LES) pressure, abdominal pressure, recurrent vomiting, alcohol use,
overweight, or smoking. Cancer of the esophagus and silent aspiration may be
life-threatening for those with gastroesophageal reflux disease (GERD).
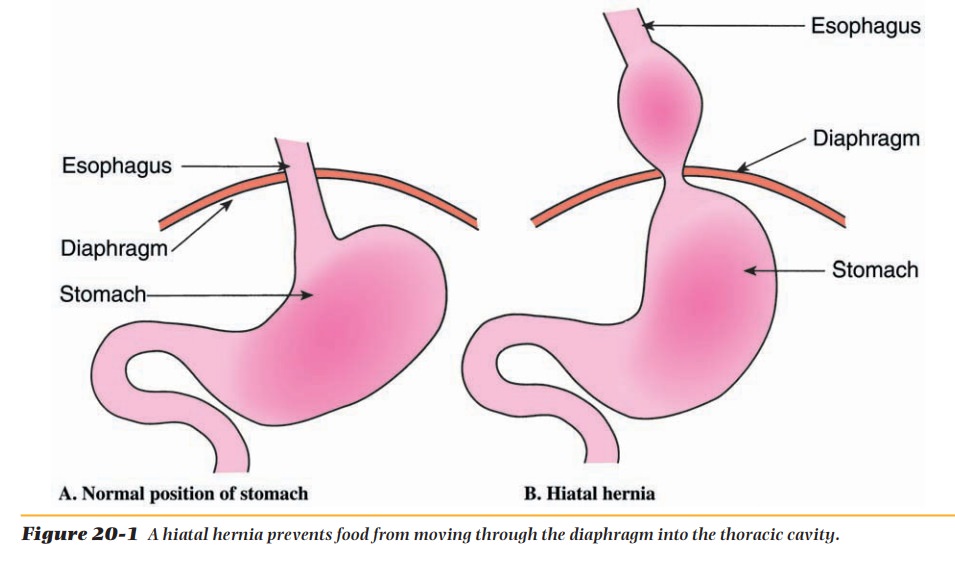
Hiatal Hernia
Hiatal hernia is a condition in
which a part of the stomach protrudes throughthe diaphragm into the thoracic
cavity (Figure 20-1). The hernia prevents the food from moving normally along
the digestive tract, although the food does mix somewhat with the gastric
juices. Sometimes the food will move back into the esophagus, creating a
burning sensation (heartburn), and sometimes food will be regurgitated into the
mouth. This condition can be very uncomfortable.
Medical Nutrition Therapy.The symptoms can
sometimes be alle-viated by serving small, frequent meals (from a well-balanced
diet) so that the amount of food in the stomach is never large. Avoid irritants
to the esophagus such as carbonated beverages, citrus fruits and juices, tomato
products, spicy foods, coffee, pepper, and some herbs. Some foods can cause the
lower esopha-geal sphincter to relax, and these should be avoided. Examples are
alcohol, garlic, onion, oil of peppermint and spearmint, chocolate, cream
sauces, gravies, margarine, butter, and oil. If the client is obese, weight
loss may be recommended to reduce pressure on the abdomen. It may also be
helpful if
When they do
lie down, they may be more comfortable sleeping with their heads and upper
torso somewhat elevated and wearing loose-fitting clothing. If discomfort cannot
be controlled, surgery may be necessary.
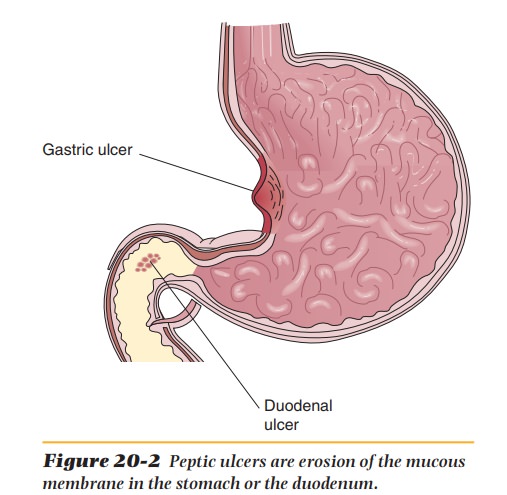
Peptic Ulcers
An ulcer is an erosion
of the mucous membrane (Figure 20-2). Peptic
ulcers may occur in the stomach (gastric
ulcer) or the duodenum (duodenalulcer). The specific cause of
ulcers is not clear, but some physicians believethat a number of factors
including genetic predisposition, abnormally high secretion of hydrochloric
acid by the stomach, stress, excessive use of aspirin or ibuprofen
(analgesics), cigarette smoking, and, in some cases, a bacterium called Helicobacter pylori may contribute to
their development.
A classic symptom is
gastric pain, which is sometimes described as burning, and in some cases,
hemorrhage is also a symptom. The pain is typi-cally relieved with food or
antacids. A hemorrhage usually requires surgery.
Ulcers are generally
treated with drugs such as antibiotics and cimeti-dine. The antibiotics kill
the bacteria, and cimetidine inhibits acid secretion in the stomach and thus
helps to heal the ulcer. Antacids containing calcium carbonate can also be
prescribed to neutralize any excess acid. Stress manage-ment may also be
beneficial in the treatment of ulcers.
Sufficient low-fat
protein should be provided but not in excess because of its ability to
stimulate gastric acid secretion. It is recommended that clients receive no
less than 0.8 gram of protein per kilogram of body weight. However, if there
has been blood loss, protein may be increased to 1 or 1.5 grams per kilogram of
body weight. Vitamin and mineral supplements, especially iron if there has been
hemorrhage, may be prescribed.
Although fat inhibits
gastric secretions, because of the danger of athero-sclerosis, the amount of
fat in the diet should not be excessive. Carbohydrates have little effect on
gastric acid secretion.
Spicy foods may be
eaten as tolerated. Coffee, tea, or anything else that contains caffeine or
that seems to cause indigestion in the client or stimulates gastric secretion
should be avoided. Alcohol and aspirin irritate the mucous membrane of the
stomach, and cigarette smoking decreases the secretion of the pancreas that
buffers gastric acid in the duodenum. Currently, a well-balanced diet of three
meals a day consisting of foods that do not irritate the client is generally
recommended.
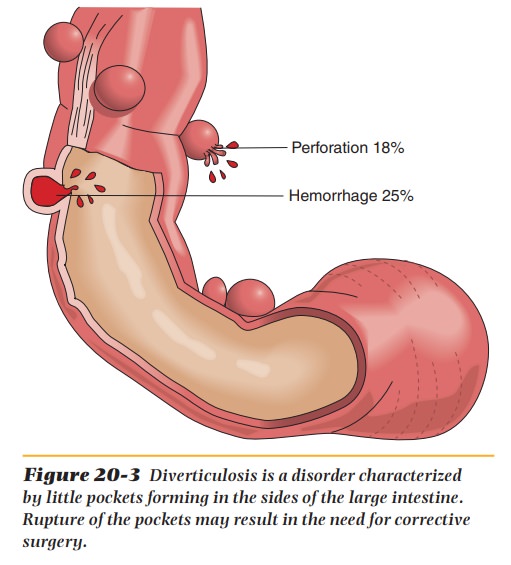
Diverticulosis/Diverticulitis
Diverticulosis is an intestinal
disorder characterized by little pockets in thesides of the large intestine
(colon) (Figure 20-3). When fecal matter collects in these pockets instead of
moving on through the colon, bacteria may breed, and inflammation and pain can
result, causing diverticulitis. If a diverticulum
ruptures, surgery may be needed. This condition is thought to be caused by a
diet lacking sufficient fiber. A high-fiber diet is commonly recommended for
clients with diverticulosis.
Along with
antibiotics, diet therapy for diverticulitis may begin with a clear liquid
diet, followed by a low-residue diet that allows the bowel to rest and heal.
Then a high-fiber diet will be a initiated. The bulk provided by the high-fiber
diet increases stool volume, reduces the pressure in the colon, and shortens
the time the food is in the intestine, giving bacteria less time to grow.
Inflammatory Bowel Disease
Inflammatory bowel diseases (IBDs) are chronic conditions
causing inflam-mation in the gastrointestinal tract. The inflammation causes
malabsorption that often leads to malnutrition. The acute phases of these
diseases occur at irregular intervals and are followed by periods in which
clients are relatively free of symptoms. Neither cause nor cure for these
conditions is known.
Two examples are ulcerative colitis and Crohn’s disease (Table 20-1).
Ulcerative colitis causes inflammation and ulceration of the colon, the rectum,
or sometimes the entire large intestine. Crohn’s disease is a chronic
progres-sive disorder that can affect both the small and large intestines. The
ulcers can penetrate the entire intestinal wall, and the chronic inflammation
can thicken the intestinal wall, causing obstruction.
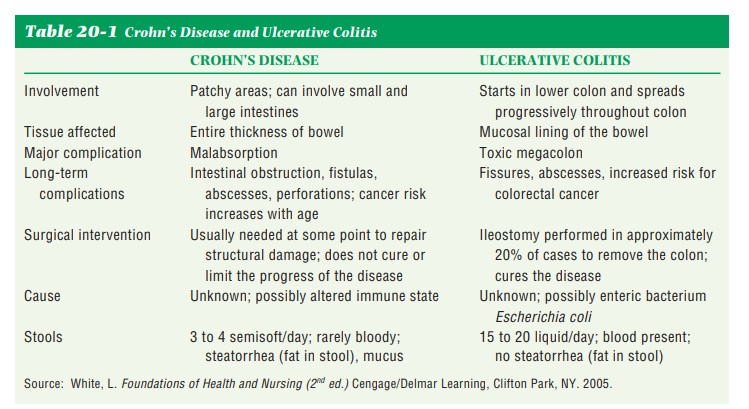
Both conditions cause
bloody diarrhea, cramps, fatigue, nausea, anorexia, malnutrition, and weight
loss. Electrolytes, fluids, vitamins, and other minerals are lost in the
diarrhea, and the bleeding can cause loss of iron and protein.
Treatment may involve anti-inflammatory drugs plus medical nutri-tion therapy. Usually a low-residue diet is required to avoid irritating the inflamed area and to avoid the danger of obstruction.
When tolerated, the diet should include about
100 grams of protein, additional calories, vitamins, and minerals.
In severe cases, total parenteral nutrition (TPN) (a process in which
nutrients are delivered directly into the superior vena cava;) may be necessary
for a period. As the client begins to regain health, the diet may be
increasingly liberalized to suit the client’s tastes while maintaining good
nutrition.
Ileostomy or Colostomy
Clients with severe
ulcerative colitis or Crohn’s disease frequently require a surgical opening
from the body surface to the intestine for the purpose of defecation. The
opening that is created is called a stoma and is about the size
of a nickel. An ileostomy (from the ileum to
abdomen surface) is required when the entire colon, rectum, and anus must be
removed. A colostomy (from the colon to
abdomen surface) can provide entrance into the colon if the rectum and anus are
removed. This can be a temporary or a permanent procedure.
Clients with
ileostomies have a greater-than-normal need for salt and water because of
excess losses. A vitamin C supplement is recommended and, in some cases, a B12
supplement may be needed. Eating a well-balanced indi-vidualized diet will
prevent a nutritional deficiency for clients with ileostomies and colostomies.
Celiac Disease
Celiac disease, also
called nontropical sprue or gluten
sensitivity, is a disorder characterized by malabsorption of virtually all
nutrients. It is thought to be due to heredity.
Symptoms include
diarrhea, weight loss, and malnutrition. Stools are usually foul-smelling,
light-colored, and bulky. The cause is unknown, but it has been found that the
elimination of gluten from the diet gives
relief. Untreated, it is life-threatening because of the severe malnutrition
and weight loss it can cause.
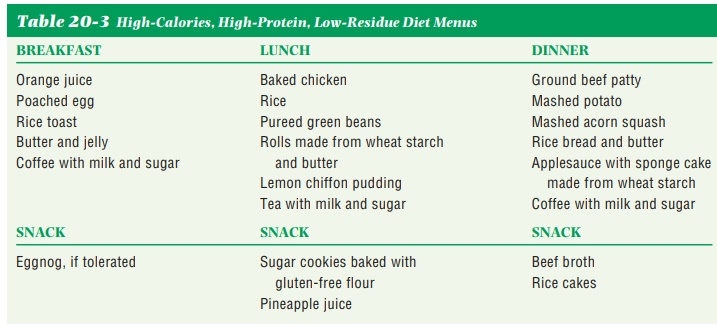
gluten-controlled diet (Table 20-2) is used in the treatment of celiac disease. Gluten is a protein found in barley, oats, rye, and wheat. All products containing these grains are disallowed.
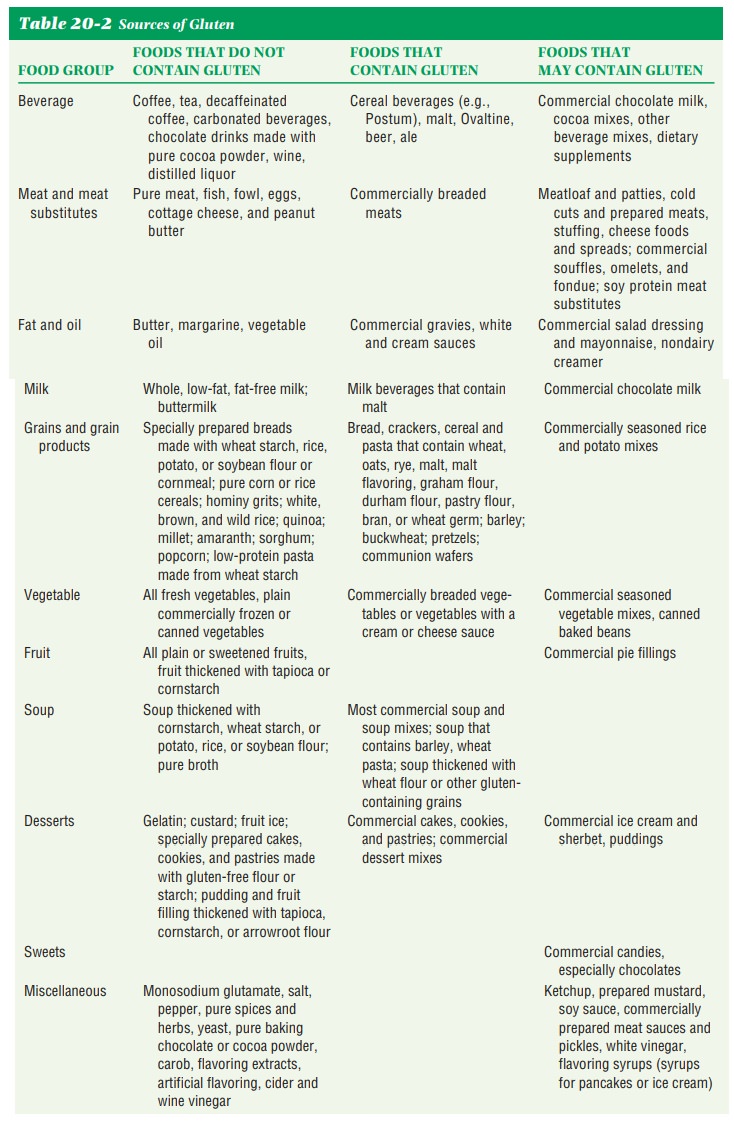
Rice and corn may be used. A reduc-tion in the fiber
content is also frequently recommended. If the client is under weight, the diet
should also be high in calories, carbohydrates, and protein (Table 20-3). Fat
may be restricted until bowel function is normalized. Vitamin and mineral
supplements may be prescribed. Lactose intolerance sometimes develops with
celiac disease.
It is not easy to
avoid food products containing wheat. Breads, cereals, crackers, pasta
products, desserts, gravies, white sauces, and beer contain wheat or other
cereal grains with gluten. The client will have to learn to read food labels
carefully and to avoid restaurant foods such as breaded meats or fish,
meatloaf, creamed vegetables, and cream soups.
Related Topics