Chapter: Clinical Cases in Anesthesia : Total Hip Replacement
Discuss thromboembolism prophylaxis and the placement of neuraxial anesthesia
Discuss thromboembolism prophylaxis and the placement of neuraxial
anesthesia.
It is common practice for orthopedists to
anticoagulate patients after total joint surgery to prevent thromboembolic
events. This is accomplished with a multitude of medications such as
unfractionated heparin, low-molecular-weight heparin (LMWH), warfarin, and
newer agents such as thrombin inhibitors and fondaparinux. All these
medica-tions can place the patient at risk for epidural hematoma if a neuraxial
anesthetic is performed.
The American Society of Regional Anesthesia
(ASRA) published guidelines in 2002 regarding neuraxial anes-thesia in the
anticoagulated patient. Patients who receive subcutaneous heparin can safely
receive neuraxial anesthe-sia, although it is probably better to delay heparin
adminis-tration until after the block is performed. In addition, if the patient
has received subcutaneous heparin for 4 or more days, a platelet count should
be done prior to performing a neuraxial anesthetic and before catheter removal.
Patients on LMWH should not have neuraxial
anesthe-sia performed until 12 hours after the last dose. For those who receive
twice-daily dosing, LMWH should not be administered until 24 hours after
surgery.
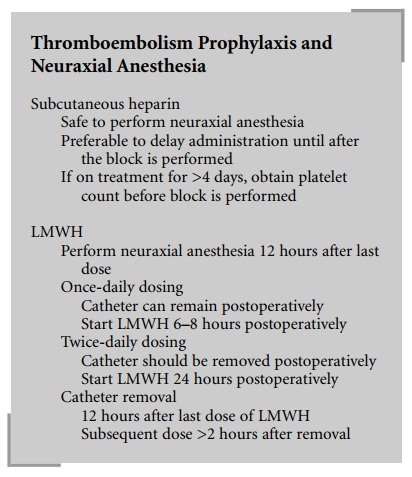
Epidural catheters should not remain in these patients
and LMWH should not be administered until 2 hours after catheter removal. Those
who receive single daily dosing can have a catheter safely maintained, and the
first dose should begin 6–8 hours postoperatively. Catheters should not be
removed until 12 hours after the last LMWH dose and the subsequent dose should
not be given until 2 hours after catheter removal.
Those patients who will be initiating warfarin
therapy more than 24 hours prior to surgery should have their International
Normalized Ratio (INR) assessed. There are no guidelines given by the ASRA for
an actual INR ratio below which neuraxial anesthesia can be safely performed,
but 1.4 is a commonly agreed upon number. Those patients on chronic warfarin
therapy should stop this medication 4–5 days prior to the procedure.
The ASRA guidelines comment that chronic NSAID
use is not known to increase the incidence of epidural hematoma after neuraxial
anesthesia.
There are no guidelines for the newer
anticoagulating agents, such as thrombin inhibitors and fondaparinux, as these
have not been time-tested yet. The ASRA recom-mends that the use of neuraxial
anesthesia in this setting should be done only in the course of clinical
trials.
Related Topics