Chapter: Medical Physiology: Transport of Oxygen and Carbon Dioxide in Blood and Tissue Fluids
Diffusion of Carbon Dioxide from the Peripheral Tissue Cells into the Capillaries and from the Pulmonary Capillaries into the Alveoli
Diffusion of Carbon Dioxide from the Peripheral Tissue Cells into the Capillaries and from the Pulmonary Capillaries into the Alveoli
When oxygen is used by the cells, virtually all of it becomes carbon dioxide, and this increases the intra-cellular PCO2; because of this high tissue cell PCO2, carbon dioxide diffuses from the cells into the tissue capillaries and is then carried by the blood to the lungs. In the lungs, it diffuses from the pulmonary capillaries into the alveoli and is expired.
Thus, at each point in the gas transport chain, carbon dioxide diffuses in the direction exactly opposite to the diffusion of oxygen. Yet there is one major difference between diffusion of carbon dioxide and of oxygen: carbon dioxide can diffuse about 20 times as rapidly as oxygen. Therefore, the pressure differences required tocause carbon dioxide diffusion are, in each instance, far less than the pressure differences required to cause oxygen diffusion. The CO2 pressures are approxi-mately the following:
1. Intracellular PCO2, 46 mm Hg; interstitial PCO2, 45 mm Hg. Thus, there is only a 1 mm Hg pressure differential, as shown in Figure 40–5.
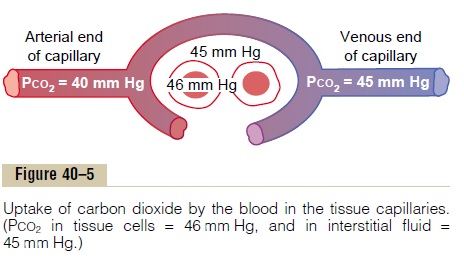
2. PCO2 of the arterial blood entering the tissues, 40 mm Hg; PCO2 of the venous blood leaving the tissues, 45 mm Hg. Thus, as shown in Figure 40–5, the tissue capillary blood comes almost exactly to equilibrium with the interstitial PCO2 of 45 mm Hg.
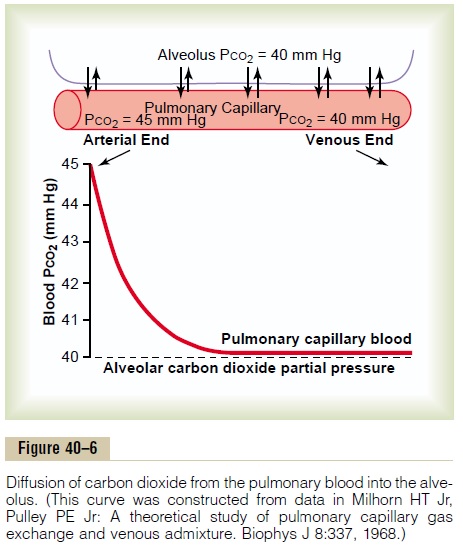
3. PCO2 of the blood entering the pulmonary capillaries at the arterial end, 45 mm Hg; PCO2 of the alveolar air, 40 mm Hg. Thus, only a 5 mm Hg pressure difference causes all the required carbon dioxide diffusion out of the pulmonary capillaries into the alveoli. Furthermore, as shown in Figure 40–6, the PCO2 of the pulmonary capillary blood falls to almost exactly equal the alveolar PCO2 of 40 mm Hg before it has passed more than about one third the distance through the capillaries. This is the same effect that was observed earlier for oxygen diffusion, except that it is in the opposite direction.
Effect of Rate of Tissue Metabolism and Tissue Blood Flow on Interstitial PCO2. Tissue capillary blood flow and tissuemetabolism affect the PCO2 in ways exactly opposite to their effect on tissue PO2. Figure 40–7 shows these effects, as follows:
1. A decrease in blood flow from normal (point A) to one quarter normal (point B) increases peripheral tissue PCO2 from the normal value of 45 mm Hg to an elevated level of 60 mm Hg.
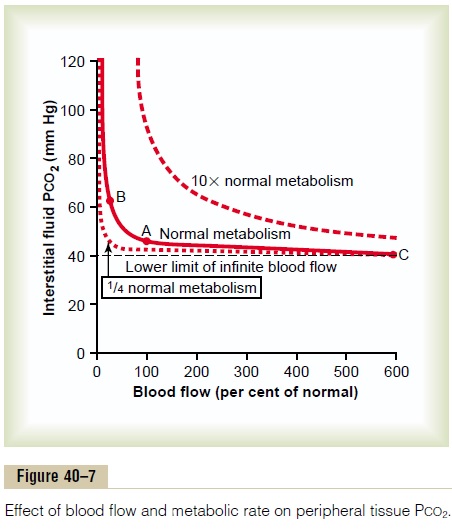
Conversely, increasing the blood flow to six times normal (point C) decreases the interstitial PCO2 from the normal value of 45 mm Hg to 41 mm Hg, down to a level almost equal to the PCO2 in the arterial blood (40 mm Hg) entering the tissue capillaries.
2. Note also that a 10-fold increase in tissue metabolic rate greatly elevates the interstitial fluid PCO2 at all rates of blood flow, whereas decreasing the metabolism to one quarter normal causes the interstitial fluid PCO2 to fall to about 41 mm Hg, closely approaching that of the arterial blood, 40 mm Hg.
Related Topics