Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Diagnostic Evaluation - Vascular Disorders
Diagnostic Evaluation
In
identifying and diagnosing the various abnormalities affecting the vascular
structures (arteries, veins, and lymphatics), various tests may be performed.
DOPPLER ULTRASOUND FLOW STUDIES
Palpating
pulses is subjective, and the examiner may mistake his or her own pulse for
that of the patient. To prevent this, the examiner should use light touch and
avoid using only the index finger for pal-pation, because this finger has the
strongest arterial pulsation of all the fingers. The thumb should not be used
for the same reason. When pulses cannot be reliably palpated, use of a
microphone-like, hand-held Doppler ultrasound device, called a transducer or
probe, may be helpful in detecting and assessing peripheral flow.
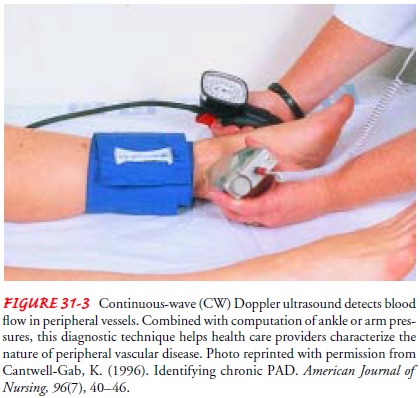
A continuous-wave
(CW) Doppler ultrasound device may be used to hear (insonate) the blood flow in
vessels when pulses can-not be palpated. This hand-held device emits a
continuous signal through the patient’s tissues. The signals are reflected by
(echo off ) the moving blood cells and are received by the device. The
filtered-output Doppler signal is then transmitted to a loudspeaker or
headphones, where it can be heard for interpretation. Because CW Doppler emits
a continuous signal, all vascular structures in the path of the sound beam are
insonated, and differentiating ar-terial from venous flow and detecting the
site of a stenosis may be difficult. The depth at which blood flow can be
detected by Doppler is determined by the frequency (in megahertz [MHz]) it
generates. The lower the frequency, the deeper the tissue penetration; a 5- to
10-MHz probe may be used to evaluate the peripheral arteries.
To evaluate the lower extremities, the patient is placed in a supine position with the head of bed elevated 20 to 30 degrees; the legs are externally rotated, if possible, to permit adequate access to the medial malleolus.
Acoustic gel is applied to the patient’s skin to
permit uniform transmission of the ultrasound wave (electro-cardiogram gel is
not used because it contains sodium, which may dissolve the epoxy that covers
the transducer’s tip). The tip of the Doppler transducer is positioned at a 45-
to 60-degree angle over the expected location of the artery and angled slowly
to identify arterial blood flow. Excessive pressure is avoided because severely
diseased arteries can collapse with even minimal pressure.
Because
the equipment can detect blood flow in advanced ar-terial disease states,
especially if collateral circulation has devel-oped, identifying a signal
documents only the presence of blood flow. However, it is clinically relevant
to notify the primary care provider of the absence of a signal if one had been
detected during a previous examination.
CW
Doppler (Fig. 31-3) is more useful as a clinical tool when combined with ankle
blood pressures, which are used to determine the ankle-brachial index (ABI), also called the ankle-arm index(AAI). The ABI is the ratio of the ankle systolic
blood pressure tothe arm systolic blood pressure. It is an objective indicator
of arte-rial disease that allows the examiner to quantify the degree of
ste-nosis. With increasing degrees of arterial narrowing, there is a
progressive decrease in systolic pressure distal to the involved sites.
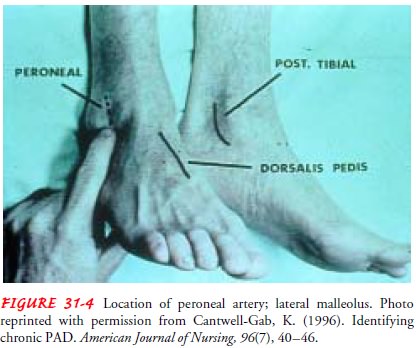
The
first step in determining the ABI is to have the patient rest in a supine
position (not seated) for at least 5 minutes. An ap-propriate-sized blood
pressure cuff (typically, a 10-cm cuff) is ap-plied to the patient’s ankle
above the malleolus. After identifying an arterial signal at the posterior
tibial and dorsalis pedis arteries, the systolic ankle pressures are obtained
in both feet. Diastolic pressures cannot be measured with a Doppler. If
pressure in these arteries cannot be measured, pressure can be measured in the
per-oneal artery, which can also be assessed at the ankle (Fig. 31-4).
Doppler
ultrasonography is used to measure brachial pressures in both arms. Both arms
are evaluated because the patient may have an asymptomatic stenosis in the
subclavian artery, causing brachial pressure on the affected side to be 20 mm
Hg or more lower than systemic pressure. The abnormally low pressure should not
be used for assessment.
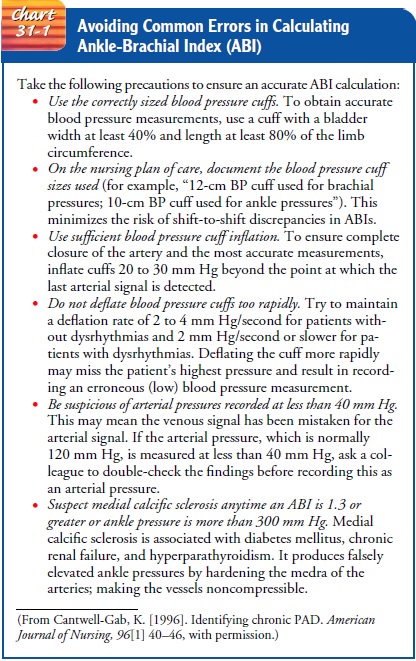
To calculate ABI, the ankle systolic pressure for each foot is divided by the higher of the two brachial systolic pressures; Chart 31-1 offers more information. The ABI can be computed for a patient with the following systolic pressures:
Right brachial: 160 mm Hg
Left brachial: 120 mm Hg
Right posterior tibial: 80 mm Hg
Right dorsalis pedis: 60 mm Hg
Left posterior tibial: 100 mm Hg
Left dorsalis pedis: 120 mm Hg
The
highest systolic pressure for each ankle (80 mm Hg for the right, 120 mm Hg for
the left) would be divided by the highest brachial pressure (160 mm Hg).
Right: 80/160 mm Hg=0.50
ABI
Left: 120/160 mm Hg=0.75
ABI
In
general, systolic pressure in the ankle of a healthy person is the same or
slightly higher than the brachial systolic pressure, resulting in an ABI of
about 1.0 (no arterial insufficiency). Pa-tients with claudication usually have
an ABI of 0.95 to 0.50 (mild to moderate insufficiency); patients with ischemic
rest pain have an ABI of less than 0.50, and patients with severe ischemia or
tissue loss have an ABI of 0.25 or less.
EXERCISE TESTING
Exercise
testing is used to determine how long a patient can walk and to measure the
ankle systolic blood pressure in response to walking. The patient walks on a
treadmill at 1.5 mph with a 10% incline for a maximum of 5 minutes. Most
patients can complete the test unless they have severe cardiac, pulmonary, or
orthopedic problems or are physically disabled. A normal response to the test
is little or no drop in ankle systolic pressure after exercise. In a pa-tient
with true claudication, however, ankle pressure drops. Com-bining this
hemodynamic information with the walking time helps the physician determine
whether intervention is necessary.
DUPLEX ULTRASONOGRAPHY
Duplex ultrasonography involves B-mode gray-scale imaging ofthe tissue, organs, and blood vessels (arterial and venous) and per-mits estimation of velocity changes by use of a pulsed Doppler (Fig. 31-5).
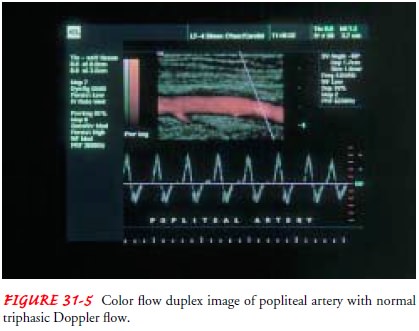
Color flow techniques, which can identify vessels, may be used to
shorten the examination time. The procedure helps determine the level and
extent of disease and is universally employed to evaluate the venous system.
The technique makes it possible to image and assess blood flow, evaluate the runoff
status of the distal vessels, locate the disease (stenosis versus occlusion),
and determine anatomic morphology and the hemodynamic sig-nificance of plaque
causing stenosis. Duplex ultrasound findings help in planning therapy and
monitoring its outcomes. More-over, the test is noninvasive and usually
requires no patient prepa-ration. The equipment is portable, making it useful
anywhere for initial diagnosis or follow-up evaluations.
COMPUTED TOMOGRAPHY
Computed
tomography (CT) provides cross-sectional images of soft tissue and can identify
the area of volume changes to an ex-tremity and the compartment where changes
take place. CT of a lymphedematous arm or leg, for example, demonstrates a
char-acteristic honeycomb pattern in the subcutaneous tissue.
In
spiral (also called volumetric) CT, the scan head moves cir-cumferentially
around the patient as the patient passes through the scanner, creating a series
of overlapping images that are con-nected to one another in a continuous spiral
(Verta & Verta, 1998). Scan times are short; however, the patient is
exposed to x-rays, and contrast agent usually must be injected to adequately
visualize the blood vessels. Using computer software, the slicelike images are
reconstructed into three-dimensional images that can be rotated and viewed from
multiple angles.
COMPUTED TOMOGRAPHIC ANGIOGRAPHY
In
computed tomographic angiography (CTA), a spiral CT scan-ner and rapid
intravenous infusion of contrast agent are used to image very thin (1-mm)
sections of the target area; the results are configured in three dimensions so
that the image closely resem-bles a regular angiogram (Verta & Verta,
1998). CTA shows the aorta and main visceral arteries better than it shows
smaller branch vessels. Scan times are usually between 20 and 30 seconds. The
large volume of contrast agent required for CTA limits the useful-ness of this
study in patients with allergy to the contrast agent or with significantly
impaired renal function.
MAGNETIC RESONANCE ANGIOGRAPHY
Magnetic resonance angiography is performed with a standard MRI scanner but with image-processing software specifically pro-grammed to isolate the blood vessels. The images are reconstructed to resemble a standard angiogram, but because the images are re-assembled in three dimensions, they can be rotated and viewed from multiple angles. Because no contrast agent is necessary, this study is useful in patients with poor renal function or allergy to contrast agent. Scan time is long, and motion artifacts are com-mon, restricting the use of the test to relatively short segments of the vascular system (Verta & Verta, 1998).
ANGIOGRAPHY
An
arteriogram produced by angiography may be used to confirm the diagnosis of
occlusive arterial disease when considering surgery or other interventions. The
procedure involves injecting a radio-paque contrast agent directly into the
vascular system to visualize the vessels. The location of a vascular
obstruction or an aneurysm (abnormal
dilation of a blood vessel) and the collateral circulation can be demonstrated.
Usually, patients experience a temporary sensation of warmth as the contrast
agent is injected, and local irritation may occur at the injection site.
Infrequently, a patient may have an immediate or delayed allergic reaction to
the iodine contained in the contrast agent. Manifestations include dyspnea,
nausea and vomiting, sweating, tachycardia, and numbness of the extremities.
Any such reaction must be reported to the physician at once; treatment may
include the administration of one or more of epinephrine (adrenaline),
antihistamines, or corticosteroids. Additional risks include vessel injury,
bleeding, and CVA (brain attack, stroke).
AIR PLETHYSMOGRAPHY
Named
for the standardized air chambers that fit around the lower leg and that are
calibrated after being filled with a standard amount of air, air
plethysmography quantifies venous reflux and calf muscle pump ejection. Changes
in volume are measured with the patient’s legs elevated, with the patient
supine and standing, and after the patient performs toe-ups (patient extends
ankle while standing; stands on tip-toes). Air plethysmography provides
in-formation about venous filling time, functional venous volume, ejected
volume, and residual volume. It is useful in evaluating pa-tients with
suspected valvular incompetence or chronic venous insufficiency.
CONTRAST PHLEBOGRAPHY
Also
known as venography, contrast phlebography involves in-jecting radiographic
contrast media into the venous system through a dorsal foot vein. If a thrombus
exists, the x-ray image discloses an unfilled segment of vein in an otherwise
completely filled vein. Injection of the contrast agent may cause a brief but
painful inflammation of the vein. The test is generally per-formed if the
patient is to undergo thrombolytic therapy, but duplex ultrasonography is now
accepted as the gold standard for diagnosing venous thrombosis.
LYMPHANGIOGRAPHY
Lymphangiography
affords a means of detecting lymph node in-volvement that results from
metastatic carcinoma, lymphoma, or infection in sites that are otherwise
inaccessible to the examiner except by surgery. In this test, a lymphatic
vessel in each foot (or hand) is injected with contrast agent. A series of
x-rays are taken at the conclusion of the injection, 24 hours later, and
periodically thereafter, as indicated. The failure to identify subcutaneous
lym-phatic collection of contrast agent and the persistence of contrast agent
in the tissue for days afterward help to confirm a diagnosis of lymphedema.
LYMPHOSCINTIGRAPHY
Lymphoscintigraphy
is a reliable alternative to lymphangiogra-phy. A radioactively labeled colloid
is injected subcutaneously in the second interdigital space. The extremity is
then exercised to facilitate the uptake of the colloid by the lymphatic system,
and serial images are obtained at preset intervals. No adverse reactions have
been reported.
Related Topics