Chapter: Essentials of Anatomy and Physiology: Blood
Diagnostic Blood Tests
DIAGNOSTIC BLOOD TESTS
Type and Cross match
To prevent transfusion reactions, the blood must be typed. Bloodtyping determines the ABO and Rh blood groups of a bloodsample. Typically, the cells are separated from the serum and then tested with known antibodies to determine the type of antigen on the cell surface. For example, if a patient’s blood cells agglutinate when mixed with anti-A antibodies but do not agglutinate when mixed with anti-B antibodies, the cells have type A antigen. In a similar fashion, the serum is mixed with known cell types (anti-gens) to determine the type of antibodies in the serum.
Normally, donor blood must match the ABO and Rh type of the recipient. However, because other blood groups can cause a transfusion reaction, a crossmatch is performed. In a crossmatch, the donor’s blood cells are mixed with the recipient’s serum, and the donor’s serum is mixed with the recipient’s cells. The donor’s
Complete Blood Count
A complete blood count (CBC) is an analysis of blood that pro-vides much useful information. A CBC consists of a red blood cell count, hemoglobin and hematocrit measurements, and a white blood cell count.
Red Blood Count
Blood cell counts are usually performed electronically with a machine, but they can also be done manually with a microscope. A normal red blood count (RBC) for a male is 4.6–6.2 million red blood cells per microliter (μL) of blood; for a female, a nor-mal RBC count is 4.2–5.4 million per μL of blood. (A microliter is equivalent to 1 cubic millimeter [mm3] or 10−6 L, and one drop of blood is approximately 50 μL). The condition called eryth-rocytosis (ĕ-rith′rō-sı̄-tō′sis) is an overabundance of red bloodcells (see Clinical Impact “Erythrocytosis and Blood Doping”).
Hemoglobin Measurement
The amount of hemoglobin in a given volume of blood is usually expressed in terms of grams of hemoglobin per 100 mL of blood. The normal hemoglobin measurement for a male is 14–18 grams(g) per 100 mL of blood, and for a female 12–16 g per 100 mL of blood. An abnormally low hemoglobin measurement is an indica-tion of anemia (ă -nē ′ mē -ă ), which is either a reduced number of red blood cells or a reduced amount of hemoglobin in each red blood cell (see the Clinical Impact “Anemia” later).
Hematocrit Measurement
The percentage of the total blood volume that is composed of red blood cells is the hematocrit (h̄e ′ m̆a -t̄o -krit, hem′ a-t̄o -krit). One way to determine hematocrit is to place blood in a capillary tube and spin it in a centrifuge. The formed elements, which are heavier than the plasma, are forced to one end of the tube. Of these, the white blood cells and platelets form the buffy coat between the plasma and the red blood cells (figure 11.14). The red blood cells account for 40–52% of the total blood volume in males and 38–48% in females. The hematocrit measurement is affected by the number and size of red blood cells because it is based on volume. For example, a decreased hematocrit can result from a decreased number of normal-size red blood cells or a normal number of small red blood
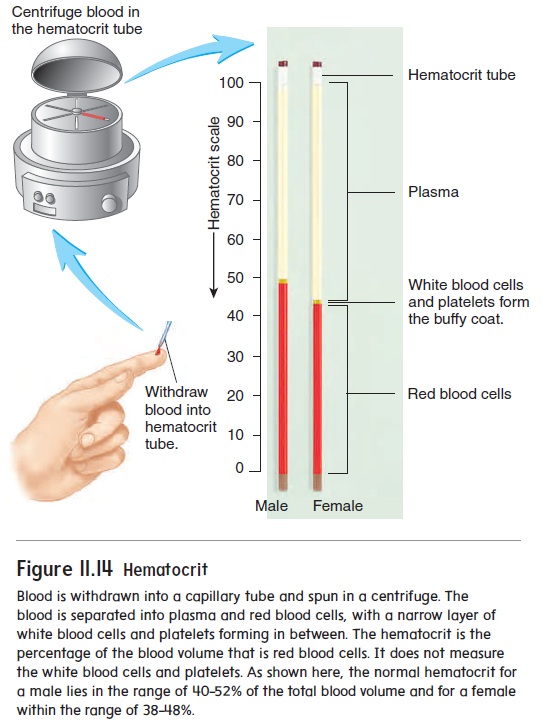
Figure 11.14 Hematocrit
cells. The average size of a red blood cell is calculated by dividing the hematocrit by the red blood cell count. A number of disorders cause red blood cells to be smaller or larger than normal. For exam-ple, inadequate iron in the diet can impair hemoglobin production. Consequently, red blood cells do not fill up with hemoglobin during their formation, and they remain smaller than normal.
White Blood Count
A white blood count (WBC) measures the total number of white blood cells in the blood. There are normally 5000–9000 white blood cells per microliter of blood. Leukopenia (loo-k̄o -p̄e ′ n̄e -̆a ) is a lower than normal WBC resulting from decreased production or destruction of the red marrow. Radiation, drugs, tumors, viral infections, or a deficiency of the vitamins folate or B12 can cause leukopenia.Leukocytosis (loo′ k̄o -s -t̄o ′ sis) is an abnormally highWBC. Bacterial infections often cause leukocytosis by stimulat-ing neutrophils to increase in number. Leukemia (loo-k̄e ′ m̄e -̆a ), cancer of the red marrow characterized by abnormal production of one or more of the white blood cell types, can cause leukocytosis. However, the white blood cells do not function normally. Because these cells are usually immature or abnormal and lack normal immunological functions, people with leukemia are very suscep-tible to infections. The excess production of white blood cells in the red marrow can also interfere with the formation of red blood cells and platelets and thus lead to anemia and bleeding.
Differential White Blood Count
A differential white blood count determines the percentage of each of the five kinds of white blood cells. Normally, neutrophils account for 60–70%, lymphocytes 20–25%, monocytes 3–8%,eosinophils 2–4%, and basophils 0.5–1% of all white blood cells. Much insight into a patient’s condition can be obtained from a dif-ferential white blood count. For example, if a bacterial infection is present, the neutrophil count is often greatly increased, whereas in allergic reactions, the eosinophil and basophil counts are elevated.
Clotting
The blood’s ability to clot can be assessed by the platelet count and the prothrombin time measurement.
Platelet Count
A normal platelet count is 250,000–400,000 platelets per microliter of blood. In the condition called thrombocytopenia (throm′ bō-sı̄-tō-pē′ nē-ă), the platelet count is greatly reduced, resulting in chronic bleeding through small vessels and capillaries. It can be caused by decreased platelet production as a result of hereditary disorders, lack of vitamin B12 (pernicious anemia), drug therapy, or radiation therapy.
Prothrombin Time Measurement
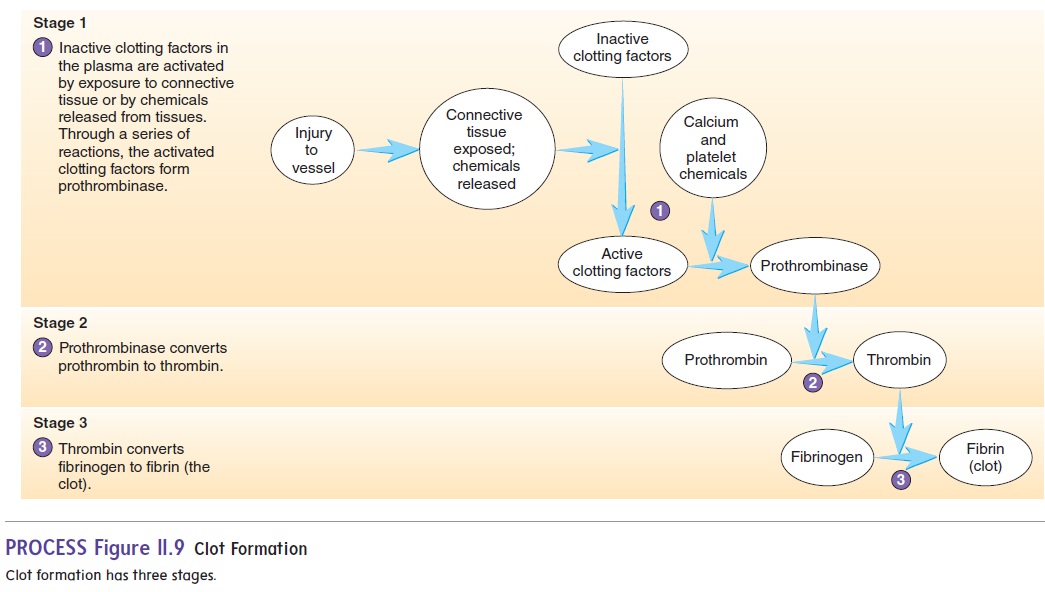
Prothrombin time measurement calculates how long it takesfor the blood to start clotting, which is normally 9–12 seconds. Prothrombin time is determined by adding thromboplastin to whole plasma. Thromboplastin is a chemical released from injured tissues that starts the process of clotting (see figure 11.9). Prothrombin time is officially reported as the International Normalized Ratio (INR), which standardizes the time it takes to clot on the basis of the slight-ly different thromboplastins used by different labs. Because many clotting factors have to be activated to form fibrin, a deficiency of any one of them can cause the prothrombin time to be abnormal. Vitamin K deficiency, certain liver diseases, and drug therapy can increase prothrombin time.
Blood Chemistry
The composition of materials dissolved or suspended in the plasma can be used to assess the functioning of many of the body’s sys-tems. For example, high blood glucose levels can indicate that the pancreas is not producing enough insulin; high blood urea nitrogen (BUN) is a sign of reduced kidney function; increased bilirubin can indicate liver dysfunction; and high cholesterol levels can signify an increased risk of cardiovascular disease. A number of blood chemistry tests are routinely done when a blood sample is taken, and additional tests are available.
Related Topics