Chapter: Clinical Dermatology: Diagnosis of skin disorders
Diagnosis of skin disorders: Examination
Examination
To examine the skin properly, the lighting must be uniform and bright. Daylight is best. The patient should usually undress so that the whole skin can be examined, although sometimes this is neither desirable (e.g. hand warts) nor possible.
The presence of a chaperone, ideally a nurse or a relative, is often sensible, and is essential if examination of the genitalia is necessary. Do not be put off this too easily by the elderly, the stubborn, the shy, or the surroundings.
Sometimes make-up
must be washed off or wigs removed. There is nothing more embarrassing than
missing the right diagnosis because an important sign has been hidden.
Distribution
A
dermatological diagnosis is based both on the distribution of lesions and on
their morphology and configuration. For example, an area of seborrhoeic
dermatitis may look very like an area of atopic der-matitis; but the key to
diagnosis lies in the location. Seborrhoeic dermatitis affects the scalp,
forehead, eyebrows, nasolabial folds and central chest; atopic dermatitis
typically affects the antecubital and pop-liteal fossae.
See
if the skin disease is localized, universal or sym-metrical. Depending on the
disease suggested by the morphology, you may want to check special areas, like
the feet in a patient with hand eczema, or the gluteal cleft in a patient who
might have psoriasis. Examine as much of the skin as possible. Look in the
mouth and remember to check the hair and the nails . Note negative as well as
positive findings, e.g. the way the shielded areas are spared in a
photosensitive dermatitis (see Fig. 16.7). Always keep your eyes open for
incidental skin cancers which the patient may have ignored.
Morphology
After
the distribution has been noted, next define the morphology of the primary
lesions. Many skin diseases have a characteristic morphology, but scratching,
ulceration and other events can change this. The rule is to find an early or
ŌĆśprimaryŌĆÖ lesion and to inspect it closely. What is its shape? What is its
size? What is its colour? What are its margins like? What are the surface characteristics?
What does it feel like?
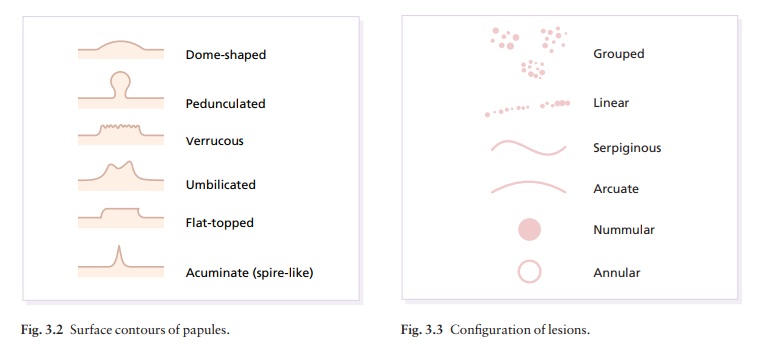
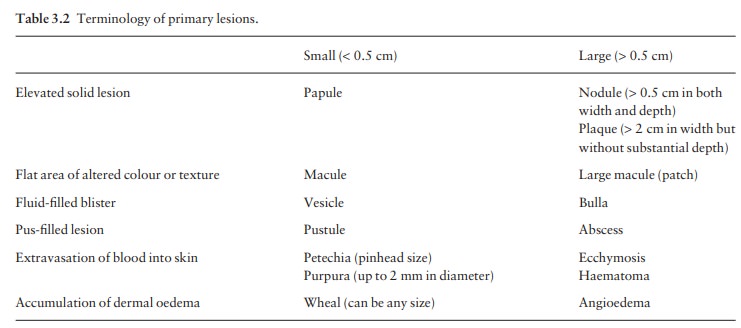
Most
types of primary lesion have one name if small, and a different one if large.
The scheme is summarized in Table 3.2.
There
are many reasons why you should describe skin diseases properly.
ŌĆó
Skin disorders are often grouped by
their morpho-logy. Once the morphology is clear, a differential diagnosis comes
easily to mind.
ŌĆó
If you have to describe a condition
accurately, you will have to look at it carefully.
ŌĆó
You can paint a verbal picture if
you have to refer the patient for another opinion.
ŌĆó
You will sound like a physician and
not a homoeopath.
ŌĆó
You will be able to understand the
terminology of this book.
Terminology of lesions (Fig. 3.1)
Primary lesions
Erythema is
redness caused by vascular dilatation.
A
papule
is a small solid elevation of skin, less than
0.5
cm in diameter.
A
plaque
is an elevated area of skin greater than
2
cm in diameter but without substantial depth.
A
macule
is a small flat area of altered colour or texture.
A
vesicle
is a circumscribed elevation of skin, less than 0.5 cm in diameter, and
containing fluid.
A
bulla
is a circumscribed elevation of skin over 0.5 cm in diameter and containing
fluid.
A
pustule
is a visible accumulation of pus in the skin.
An
abscess
is a localized collection of pus in a cavity, more than 1 cm in diameter.
Abscesses are usually nodules, and the term ŌĆśpurulent bullaŌĆÖ is some-times used
to describe a pus-filled blister that is situated on top of the skin rather
than within it.
A
wheal
is an elevated white compressible evanes-cent area produced by dermal oedema.
It is often surrounded by a red axon-mediated flare. Although usually less than
2 cm in diameter, some wheals are huge.
Angioedema
is a diffuse swelling caused by oedemaextending to the
subcutaneous tissue.
A
nodule
is a solid mass in the skin, usually greater than 0.5 cm in diameter, in both
width and depth, which can be seen to be elevated or can be palpated.
A
tumour
is harder to define as the term is based more correctly on microscopic
pathology than on clinical morphology. We keep it here as a convenient term to
describe an enlargement of the tissues by normal or pathological material or
cells that form a mass, usually more than 1 cm in diameter. Because the word
ŌĆśtumourŌĆÖ can scare patients, tumours may courteously be called ŌĆślarge nodulesŌĆÖ,
especially if they are not malignant.
A
papilloma
is a nipple-like projection from the skin.
Petechiae
are pinhead-sized macules of blood in theskin.
The
term purpura
describes a larger macule or papule of blood in the skin. Such blood-filled
lesions do not blanch if a glass lens is pushed against them (diascopy).
An
ecchymosis
is a larger extravasation of blood into the skin.
A
haematoma
is a swelling from gross bleeding.
A
burrow
is a linear or curvilinear papule, with some scaling, caused by a scabies mite.
A
comedo
is a plug of greasy keratin wedged in a dilated pilosebaceous orifice. Open
comedones are blackheads. The follicle opening of a closed comedo is nearly
covered over by skin so that it looks like a pinhead-sized, ivory-coloured
papule.
Telangiectasia
is the visible dilatation of smallcutaneous blood vessels.
Poikiloderma
is a combination of atrophy, reticu-late hyperpigmentation
and telangiectasia.
Secondary lesions
These
evolve from primary lesions.
A
scale
is a flake arising from the horny layer.
A
keratosis
is a horn-like thickening of the stratum corneum.
A
crust
may look like a scale, but is composed of dried blood or tissue fluid.
An
ulcer
is an area of skin from which the whole of the epidermis and at least the upper
part of the dermis has been lost. Ulcers may extend into subcutaneous fat, and
heal with scarring.
An
erosion
is an area of skin denuded by a complete or partial loss of only the epidermis.
Erosions heal without scarring.
An
excoriation
is an ulcer or erosion produced by scratching.
A
fissure
is a slit in the skin.
A
sinus
is a cavity or channel that permits the escape of pus or fluid.
A
scar
is a result of healing, where normal struc-tures are permanently replaced by
fibrous tissue.
Atrophy is
a thinning of skin caused by diminutionof the epidermis, dermis or subcutaneous
fat. When the epidermis is atrophic it may crinkle like cigarette paper, appear
thin and translucent, and lose normal surface markings. Blood vessels may be
easy to see in both epidermal and dermal atrophy.
Lichenification
is an area of thickened skin withincreased markings.
A
stria
(stretch mark) is a streak-like linear atrophic pink, purple or white lesion of
the skin caused by changes in the connective tissue.
Pigmentation,
either more or less than surroundingskin, can develop after lesions heal.
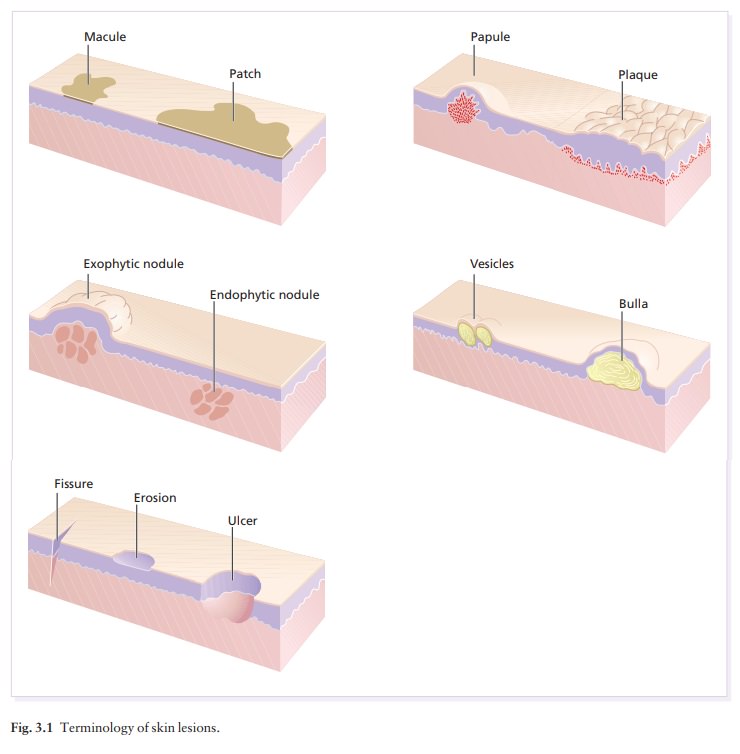
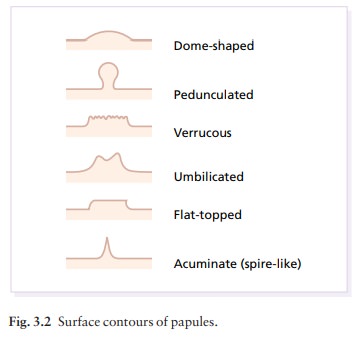
Having
identified the lesions as primary or secondary, adjectives can be used to
describe them in terms of their other features.
ŌĆó
Colour (e.g. salmon-pink, lilac,
violet).
ŌĆó
Sharpness of edge (e.g.
well-defined, ill-defined).
ŌĆó
Surface contour (e.g. dome-shaped,
umbilicated, spire-like; Fig. 3.2).
ŌĆó
Geometric shape (e.g. nummular,
oval, irregular, like the coast of Maine).
ŌĆó
Texture (e.g. rough, silky, smooth,
hard).
ŌĆó
Smell (e.g. foul-smelling).
ŌĆó
Temperature (e.g. hot, warm).
Dermatologists also
use a few
special adjectives
which
warrant definition.
ŌĆó
Nummular means round or coin-like.
ŌĆó
Annular means ring-like.
ŌĆó
Circinate means circular.
ŌĆó
Arcuate means curved.
ŌĆó
Discoid means disc-like.
ŌĆó
Gyrate means wave-like.
ŌĆó
Retiform and reticulate mean
net-like.
To
describe a skin lesion, use the term for the primary
lesion
as the noun, and the adjectives mentioned above to define it. For example, the
lesions of psoriasis may appear as ŌĆśsalmon-pink sharply demarcated nummular
plaques covered by large silver polygonal scalesŌĆÖ.
Try not to use the terms ŌĆślesionŌĆÖ or ŌĆśareaŌĆÖ. Why say ŌĆśpapular lesionŌĆÖ when you can say papule?
It is almost
as bad as the ubiquitous term ŌĆśskin rashŌĆÖ. By the way, there are very few
diseases that are truly ŌĆśmaculopapularŌĆÖ. The term is best avoided except to
describe some drug eruptions and viral exanthems. Even then, the terms
ŌĆśscarlatiniformŌĆÖ (like scarlet fever apunctate, slightly elevated papules) or
ŌĆśmorbilliformŌĆÖ (like measlesaa net-like blotchy slightly elevated pink
exanthem) are more helpful.
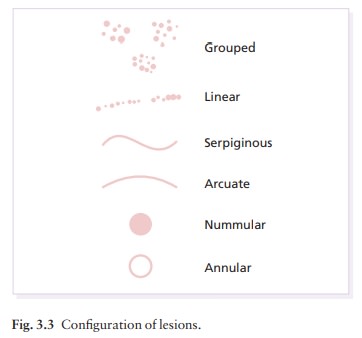
Configuration
After
unravelling the primary and secondary lesions, look for arrangements and
configurations that can be, for example, discrete, confluent, grouped, annular,
arcuate or dermatomal (Fig. 3.3). Note that while individual lesions may be
annular, several individual lesions may arrange themselves into an annular
con-figuration. Terms like annular, and other adjectives discussed under the
morphology of individual lesions, can apply to their groupings too. The K├Čbner
or iso-morphic phenomenon is the induction of skin lesions by, and at the site
of, trauma such as scratch marks or operative incisions.
Related Topics