Chapter: Medicine Study Notes : Endocrine and Electrolytes
Diabetes Mellitus
Diabetes Mellitus
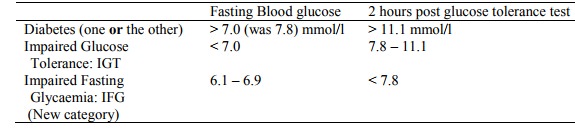
Diagnosis of diabetes
· 1999 criteria (ie textbooks out of date):
· For Diabetes:
o For Gestational Diabetes:
§ Screening: at 28 weeks, non-fasting glucose load of 50g. If >= 7.8
should have gestational glucose tolerance test
§ Gestational Glucose tolerance test: 75 g load when fasting. Fasting
level >= 5.5 OR 1 hour post glucose load of >= 11 OR 2 hour post glucose
load of >= 8.5 (some say 9.0) Ăž gestational diabetes.
§ 1 – 3 % of pregnancies have gestational diabetes
·
Suggested regime for Screening
for type 2 diabetes (Screening for type 2 diabetes, NZMJ 26 April 2002)
o Test if > 5% of diabetes Ăž Europeans over 50 and
non-Europeans > 40 years of age
o Yearly screening for anyone found to have IGT or IFG
o Best to test with morning fasting glucose – although use random test
with caution if conditions approach fasting or post-glucose load conditions
o Finger prick testing not accurate enough
o HBA1c not recommended for screening: different methods for testing and
different normal ranges
IDDM – Type 1 (Juvenile Onset Diabetes)
·
A chronic, progressive autoimmune
process in genetically susceptible people, triggered by environmental factors
·
Eventually cannot survive without
insulin treatment. Ketoacidosis will develop unless insulin given (if any
endogenous insulin then no ketones)
·
Incidence up to 20 yrs: 10 –
15/100,000
·
Prevalence: 0.25 – 3 % (10 – 15%
of all diabetics)
·
Peak age of incidence is 12 – but
can present at any age (even after 40). Surges in presentation at 3- 4,
starting school. ?Viral exposure
·
85 – 90% have no family history,
but family history confers  risk
·
Antibodies:
o Islet Cell Antibodies: risk of IDDM  with  level of
ICA. Frequency in newly diagnosed IDDM is 65 – 85%. Frequency in population is
< 0.5%
o GAD (glutamic acid decarboxylase) antibodies: mildly specific antigenic
enzyme released from islet cells when destroyed. Can test for these in
prodromal stage
o Insulin autoantibodies
·
Acute presentation:
hyperglycaemia (polyuria when glucose > 10 mmol/l, thirst, polydypsia),
tiredness, weight loss. Also cramps, blurred vision, superficial infections. Ketoacidosis
(now rare) also has nausea, vomiting, and drowsiness
·
Kids presenting with mild
hyperglycaemia: don‟t know if they will become IDDM or are MODY
·
(Maturity Onset Diabetes Of The
Young – ie Type 2). So when start insulin replacement back titrate (after
stabilised) – type 1 may have honeymoon period until no endogenous insulin
·
Currently being investigated for
prevention in high risk individuals (ie have antibodies but not frank disease):
o Cow‟s milk avoidance until 6 months of age
o Early oral insulin therapy ® autoimmune modulation
o Nicotinamide (vitamin B) supplementation
·
Treatment goals: stable blood
sugar, prevent/monitor complications, promote normal growth and development,
maintenance of normal weight
Investigations for both Type 1 and Type 2 Diabetes
· Glucose testing
· HbA1C. Any reduction worthwhile. Target is <= 7.0. Not all willing or able to achieve this
· Ketonuria
·
24 hour urine and measure
C-peptide: a by-product of insulin production (have they any endogenous insulin
– as long as replacement insulin hasn‟t ® islet cell atrophy)
·
Fundoscopy
·
Lipids
·
BP: want diastolic < 85 and
systolic < 135 (especially for young or existing microalbuminuria)
·
Microalbuminuria:
o Nephropathy has two phases:
§ Normal blood pressure, creatinine, and urines but microalbuminuria.
§ Overt neuropathy: proteinuria, hypertension, Âcreatinine
and ÂŻ GRF
o Normal level < 20 mg/24 hours. Microalbuminuria = 30 – 300 mg/24
hours. Dipsticks detect > 150 g/l (ie insensitive)
o Microalbuminuria hard to test (needs 24 hr urine). So use albumin :
creatinine ratio. Normal < 2.8 in men, < 4.5 in females in random test
o If abnormal result then patients qualify for statins with cholesterol > 6 (normal threshold > 9)
Complications
·
Microvascular disease:
o Due to thickened walls and laying down of advanced end glycosylation
products
o Eye disease: mainly retinopathy. After 30 years 80% have background
retinopathy and 7 – 8% are blind. Also  Sorbitol ® cataracts.
o Nephropathy
o Neuropathy: peripheral and autonomic
·
Macrovascular disease:
o Coronary heart disease. Male diabetics have 2 times risk, females 4
times risk. Very high risk if other risks present (eg ÂBP,
lipids, smoking etc)
o Accelerated atherosclerosis (but lesions look the same)
·
Kidney disease:
o Diabetic Nephropathy
o Onset of diabetes leads to:
§ Functional changes: ÂGFR, Reversible albuminuria
§ Structural changes: GBM thickening, mesangial expansion
o After 30 years, 30 – 40% have nephropathy. Unlikely if hasn‟t developed
after 30 years (?some protective factors)
o Glomerular damage:
§ Nodular glomerulosclerosis. Acellular hyaline material
(Kimmelstiel-Wilson Lesion): BM proliferates (ie collagen expansion of
mesangial matrix) ® sclerosed and fibrotic due to fibroblast infiltration ® chronic
renal failure. Earliest sign is microalbuminuria, due to pores getting bigger
§ Diffuse glomerulo-sclerosis: glomerular loop obstruction ® necrosis
(seen in hypertension or any end-stage renal disease)
o Papillary necrosis: least blood supply ®
susceptible to ischaemia
o Also pyelonephritis and reflux lead to kidney damage
·
Immune deficiency: White cells
affected when glucose > 14 mmol/l
·
Neuropathy:
o Glycosylation of nerve
o Demyelination of nerve due to sorbitol accumulation in Scwhann cells ® slowed
conduction
o Peripheral sensory AND motor neuropathy (eg foot deformity, fallen
arches)
o Autonomic neuropathy leads to bladder problems, impotence,
gastroenteropathy
·
® Diabetic foot
·
Special management in surgery,
pregnancy and in intercurrent illness
Management of Diabetic Ketoacidosis or Hyperglycaemia
·
Diabetic Ketoacidosis:
o Signs: nausea, vomiting, thirst, abdominal pain, delirium, coma, acetone
fetor, hypotension, tachycardia, metabolic acidosis (Kussmaul breathing),
hyperosmolality
o Treatment:
§ ABC, oxygen
§ IV crystalloid: may need 4 – 6 L. Will be severely dehydrated due to
osmotic diuresis. Use normal saline, and reduce to hypotonic fluid once
rehydrated and glucose < 15 mmol/l or if Na > 150 mmol/l
§ Potassium 20 mmol in first 6 hours then 10 mmol/hr according to plasma
levels. If plasma K high then delay adding K until this has normalised
§ Insulin: actrapid 10 – 20 units.
Resistance to insulin may suggest sepsis, insulin antibodies
§ Monitor acidosis. May need HCO3
·
Ongoing Management of Diabetes:
o Acute symptoms are main reason for seeking treatment. But good control
is more than just keeping out of trouble. Involves significant education
o For Impaired Glucose tolerance and Impaired fasting glucose: lifestyle
change and monitoring
o Diet: ÂŻSaturated fats, low glycaemic index foods (sugar presented slower to
liver, able to convert more to glycogen). Space out CHO more evenly throughout
the day. If normal BMI and NIDDM try ¯ fats and  CHO ®may  insulin
release (BMI ~ level of insulin resistance)
o Warn about effects on blood sugars of another illness (eg „flu) ® Âblood
sugars. Requires more regular monitoring. Don‟t just stop taking insulin if not
eating.
o Insulin:
§ Use fast acting for glucose peaks following meals, and long acting for
basal rate (® suppress gluconeogenesis overnight, etc)
§ Conventional regime: twice daily with both fast and long acting
§ Intensive regime: fast acting before each meal and long acting at night
(= 4 jabs a day)
§ Diabetes Complications Control Trial (1993) examined 1441 volunteers (ie
motivated) in two groups: conventional treatment (insulin once or twice daily)
and intensive (3 or 4 times daily). Intensive therapy reduced risk in all
categories, but Âhypoglycaemia and some weight gain
o Biguanides: eg metformin. ÂInsulin sensitivity, ÂŻgluconeogenesis,
won‟t ® hypoglycaemia. Nausea, vomiting, B12 malabsorption. Not in hepatic and
renal disease or pregnancy. Not in hypoxic lung disease or cardiac disease
o Sulphonylureas: Âinsulin release from b-islet cells (Ăžmust have some left for it to work),
o ÂŻgluconeogenesis
and glycogenolysis. Can ® hypoglycaemia. Nausea, vomiting. Not in hepatic and renal disease or
pregnancy.
o Monitoring: HbA1C (normal < 6.5), daily blood sugars (before
breakfast)
·
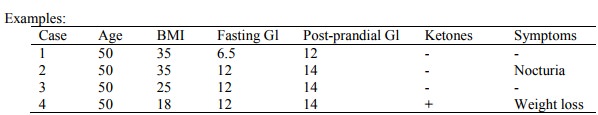
Case 1: Has more insulin than
case 2 (insulin resistance is proportional to BMI, but her glucose is
o lower Þ more insulin) Þ earlier presentation than case 2. Treatment: diet + metformin (can ®
diarrhoea secondary to malabsorption). If very overweight, check LFT
·
Case 2: pancreas starting to fail
·
Case 3: Weight loss may not do
much. Are they CHO deficient (ÂCHO ® Âinsulin release)? May start with sulphonylureas. May need insulin sooner
·
Case 4: Type 1/IDDM. Will be
catabolic – need protein. Quick test with sulphonylureas but will need insulin
at earlier stage
Related Topics