Chapter: Medical Physiology: The Autonomic Nervous System and the Adrenal Medulla
Denervation Supersensitivity of Sympathetic and Parasympathetic Organs After Denervation
Denervation Supersensitivity of Sympathetic and Parasympathetic Organs After Denervation
During the first week or so after a sympathetic or parasympathetic nerve is destroyed, the innervated organ becomes more sensitive to injected norepinephrine or acetylcholine, respectively. This effect is demon-strated in Figure 60–4, showing blood flow in the forearm before removal of the sympathetics to be about 200 ml/min; a test dose of norepinephrine causes only a slight depression in flow lasting a minute or so. Then the stellate ganglion is removed, and normal sympathetic tone is lost. At first, the blood flow rises markedly because of the lost vascular tone, but over a period of days to weeks the blood flow returns much of the way back toward normal because of progressive increase in
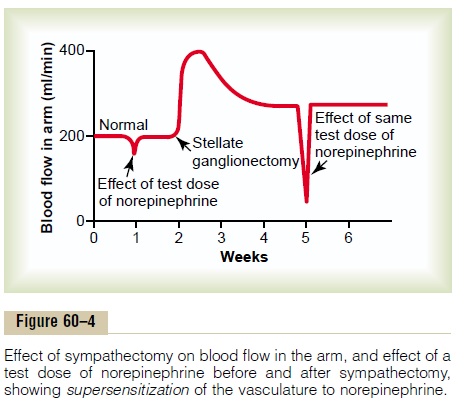
intrinsic tone of the vascular musculature itself, thus partially compensating for the loss of sympathetic tone. Then, another test dose of norepinephrine is adminis-tered, and the blood flow decreases much more than before, demonstrating that the blood vessels have become about two to four times as responsive to nor-epinephrine as previously. This phenomenon is called denervation supersensitivity. It occurs in both sympa-thetic and parasympathetic organs but to far greater extent in some organs than in others, occasionally increasing the response more than 10-fold.
Mechanism of Denervation Supersensitivity. The cause ofdenervation supersensitivity is only partially known. Part of the answer is that the number of receptors in the postsynaptic membranes of the effector cells increases—sometimes manyfold—when norepineph-rine or acetylcholine is no longer released at the synapses, a process called “up-regulation” of the recep-tors. Therefore, when a dose of the hormone is now injected into the circulating blood, the effector reaction is vastly enhanced.
Autonomic Reflexes
Many visceral functions of the body are regulated by autonomic reflexes. Throughout this text, the functionsof these reflexes are discussed in relation to individual organ systems; to illustrate their importance, a few are presented here briefly.
Cardiovascular Autonomic Reflexes. Several reflexes in thecardiovascular system help to control especially the arterial blood pressure and the heart rate. One of these is the baroreceptor reflex. Briefly, stretch receptors called baroreceptors are located in the walls of several major arteries, including especially the internal carotid arteries and the arch of the aorta. When these become stretched by high pressure, signals are transmitted to the brain stem, where they inhibit the sympathetic impulses to the heart and blood vessels and excite the parasympathetics; this allows the arterial pressure to fall back toward normal.
Gastrointestinal Autonomic Reflexes. The uppermost part ofthe gastrointestinal tract and the rectum are controlled principally by autonomic reflexes. For instance, the smell of appetizing food or the presence of food in the mouth initiates signals from the nose and mouth to the vagal, glossopharyngeal, and salivatory nuclei of the brain stem. These in turn transmit signals through the parasympathetic nerves to the secretory glands of the mouth and stomach, causing secretion of digestive juices sometimes even before food enters the mouth.
When fecal matter fills the rectum at the other end of the alimentary canal, sensory impulses initiated by stretching the rectum are sent to the sacral portion of the spinal cord, and a reflex signal is transmitted back through the sacral parasympathetics to the distal parts of the colon; these result in strong peristaltic contrac-tions that cause defecation.
Other Autonomic Reflexes. Emptying of the urinary bladderis controlled in the same way as emptying the rectum; stretching of the bladder sends impulses to the sacral cord, and this in turn causes reflex contraction of the bladder and relaxation of the urinary sphincters, thereby promoting micturition.
Also important are the sexual reflexes, which are ini-tiated both by psychic stimuli from the brain and by stimuli from the sexual organs. Impulses from these sources converge on the sacral cord and, in the male, result first in erection, mainly a parasympathetic func-tion, and then ejaculation,partially a sympathetic function.
Other autonomic control functions include reflex contributions to the regulation of pancreatic secretion, gallbladder emptying, kidney excretion of urine, sweat-ing, blood glucose concentration, and many other vis-ceral functions.
Related Topics