Chapter: Medical Surgical Nursing: Health Care Delivery and Nursing Practice
Demand for Quality Care - Influences on Health Care Delivery
DEMAND
FOR QUALITY CARE
The general public has
become increasingly interested in and knowledgeable about health care and
health promotion. This awareness has been stimulated by television, newspapers,
maga-zines, and other communications media and by political debate. The public
has become more health conscious and has in general begun to subscribe strongly
to the belief that health and quality health care constitute a basic right,
rather than a privilege for a chosen few.
In 1977, the National
League for Nursing (NLN) issued a statement on nurses’ responsibility to uphold
patients’ rights. The statement addressed patients’ rights to privacy,
confidentiality, informed participation, self-determination, and access to
health records. This statement also indicated ways in which respect for
patients’ rights and a commitment to safeguarding them could be incorporated
into nursing education programs and upheld and reinforced by those in nursing
service. Nurses can directly involve themselves in ensuring specific rights, or
they can make their in-fluence felt indirectly (NLN, 1977).
The ANA has worked
diligently to promote the delivery of quality health and nursing care. Efforts
by the ANA range from assessing the quality of health care provided to the
public in these changing times to lobbying legislators to pass bills related to
is-sues such as health insurance or length of hospital stay for new mothers.
Legislative changes have
promoted both delivery of quality health care and increased access by the
public to this care. The National Health Planning and Resources Act of 1974
empha-sized the need for planning and providing quality health care for all
Americans through coordinated health services, staffing, and facilities at the
national, state, and local levels. Medically under-served populations were the
target for the primary care services provided for by this act. By the passage
of bills supporting health insurance reform, barring discrimination against individuals
with preexisting conditions, and expanding the portability of health care
coverage, Congress has acknowledged the needs of con-sumers for adequate health
insurance in this time of longer life spans and chronic illnesses. Efforts in
some states to provide full health care coverage for citizens, particularly
children, represent measures by state governments to promote access to health
care. Legislative support of advanced practice nurses in individual practice is
a recognition of the contribution of nursing to the health of consumers,
particularly underserved populations.
Quality Improvement and Evidence-Based Practice
In the 1980s, hospitals
and other health care agencies implemented ongoing quality assurance (QA)
programs. These programs were required for reimbursement for services and for
accreditation by the Joint Commission on Accreditation of Healthcare
Organizations (JCAHO). QA programs sought to establish accountability on the
part of the health professions to society for the quality, appropri-ateness,
and cost of health services provided.
The JCAHO developed a
generic model that required moni-toring and evaluation of quality and
appropriateness of care. The model was implemented in health care institutions
and agencies through organization-wide QA programs and reporting systems.Many
aspects of the programs were centralized in a QA depart-ment. In addition, each
patient care and patient services depart-ment was responsible for developing
its own plan for monitoring and evaluation. Objective and measurable indicators
were used to monitor, evaluate, and communicate the quality and
appro-priateness of care delivered.
In the early 1990s, it
was recognized that quality of care as de-fined by regulatory agencies
continued to be difficult to measure. QA criteria were identified as measures
to ensure minimal expec-tations only; they did not provide mechanisms for
identifying causes of problems or for determining systems or processes that
need improvement. Continuous quality improvement (CQI) was identified as a more
effective mechanism for improving the qual-ity of health care. In 1992, the
revised standards of the JCAHO mandated that health care organizations
implement a CQI pro-gram. Recent amendments to JCAHO standards have specified
that patients have the right to care that is considerate and pre-serves
dignity; that respects cultural, psychosocial, and spiritual values; and that
is age specific (Krozok & Scoggins, 2001). Qual-ity improvement efforts
have focused on ensuring that the care provided meets or exceeds JCAHO
standards.
Unlike QA, which focuses
on individual incidents or errors and minimal expectations, CQI focuses on the
processes used to provide care, with the aim of improving quality by assessing
and improving those interrelated processes that most affect patient care
outcomes and patient satisfaction. CQI involves analyzing, understanding, and
improving clinical, financial, or operational processes. Problems identified as
more than isolated events are an-alyzed, and all issues that may affect the
outcome are studied. The main focus is on the processes that affect quality.
As health care agencies
continue to implement CQI, nurses have many opportunities to be involved in
quality improvement. One such opportunity is through facilitation of
evidence-based practice. Evidence-based practice—identifying and evaluating
current literature and research and incorporating the findings into care
guidelines—has been designated as a means of ensuring quality care.
Evidence-based practice includes the use of outcome assessment and standardized
plans of care such as clinical guide-lines, clinical pathways, or algorithms.
Many of these measures are being implemented by nurses, particularly by nurse
managers and advanced practice nurses. Nurses directly involved in the
de-livery of care are engaged in analyzing current data and refining the
processes used in CQI. Their knowledge of the processes and conditions that
affect patient care is critical in designing changes to improve the quality of
the care provided.
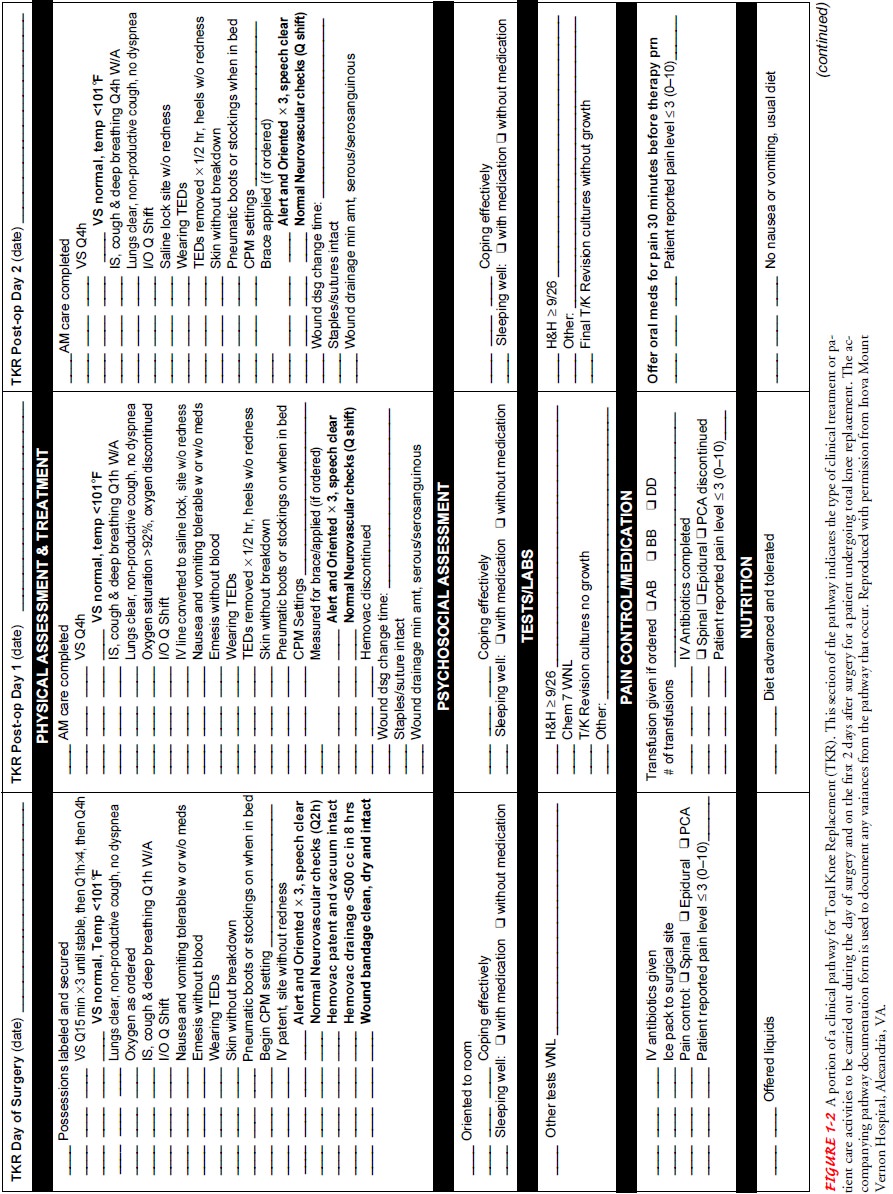
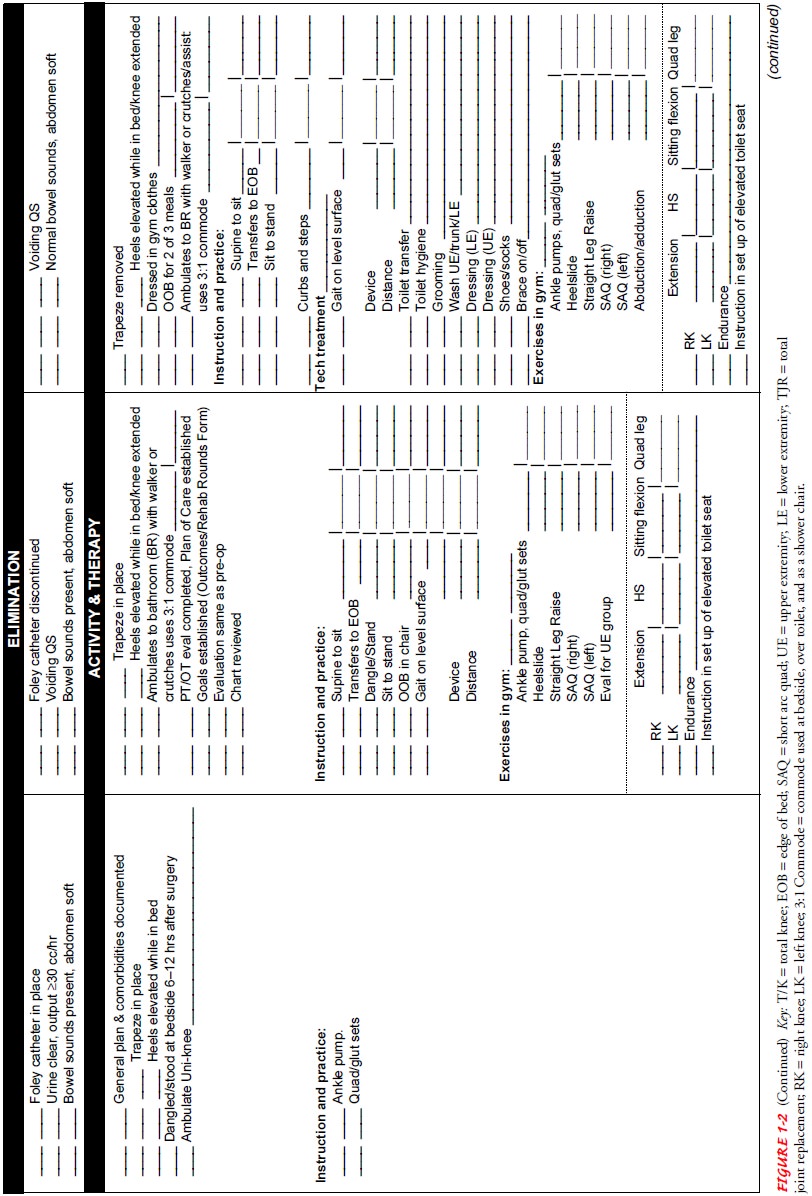
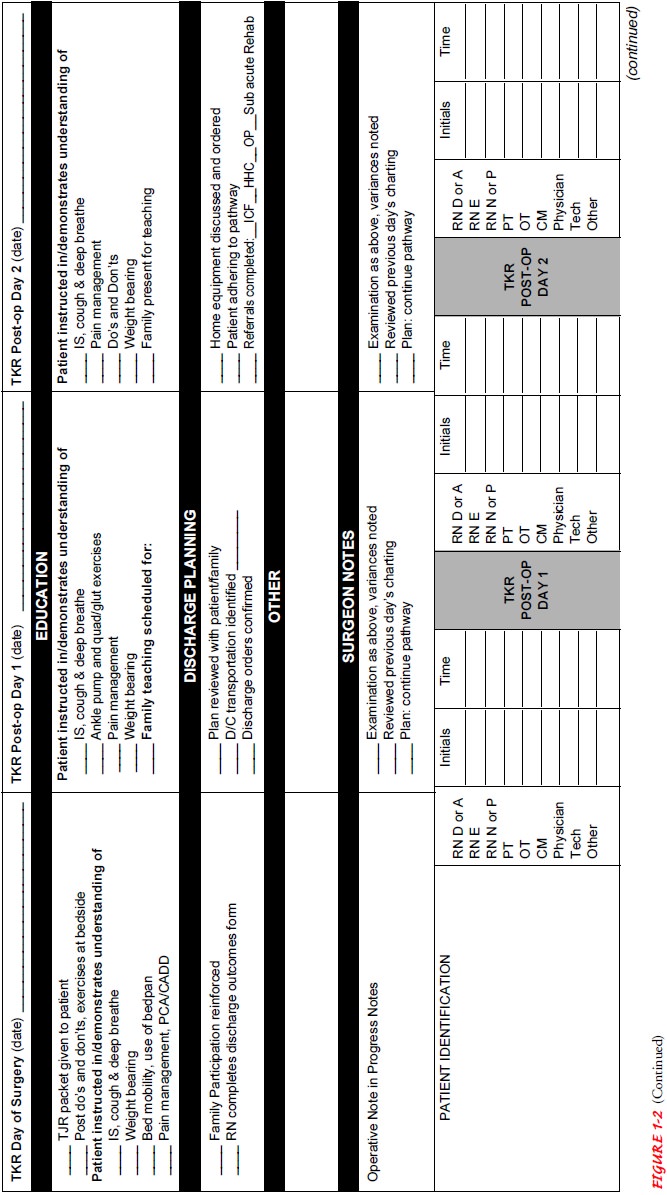
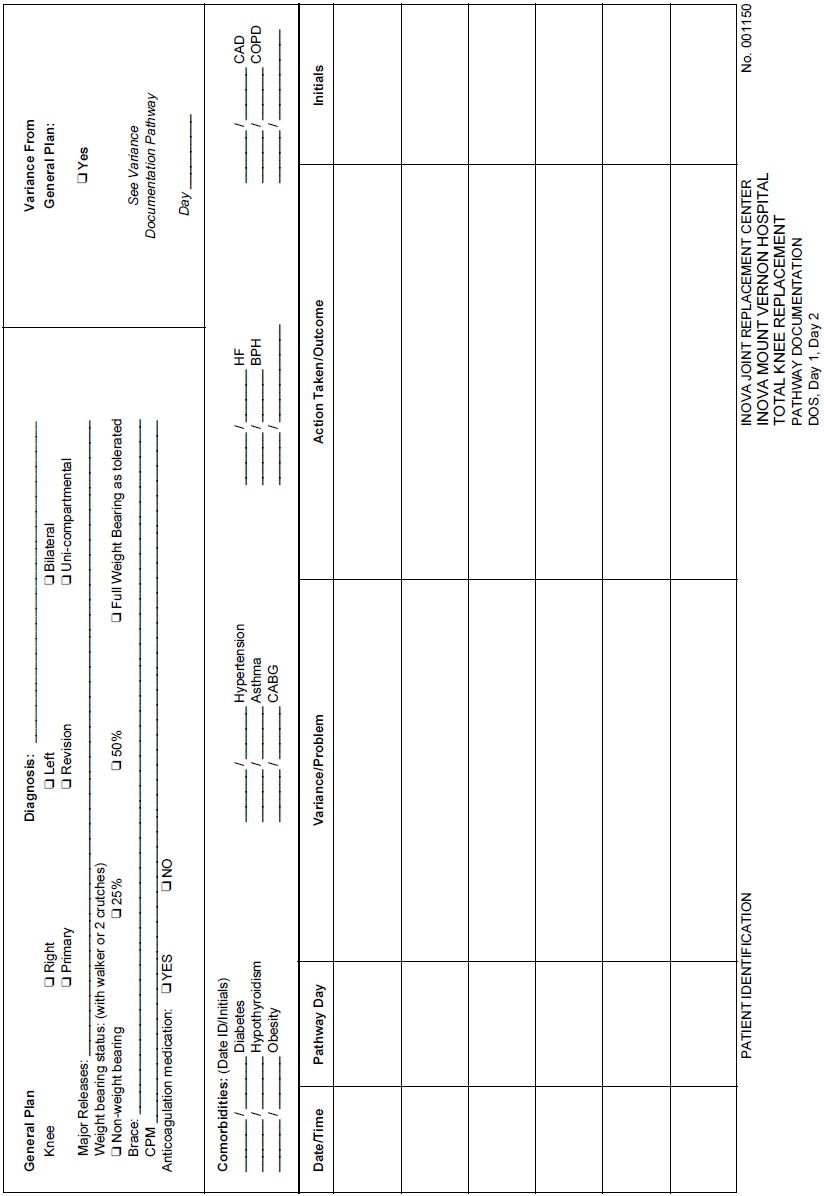
Clinical Pathways and Care Mapping
Many hospitals, managed
care facilities, and home health services nationwide use clinical pathways or
care mapping to coordinate care for a caseload of patients (Klenner, 2000).
Clinical pathways serve as an interdisciplinary care plan and as the tool for
tracking a patient’s progress toward achieving positive outcomes within
specified time frames. Clinical pathways have been developed for certain DRGs
(eg, open heart surgery, pneumonia with comor-bidity, fractured hip), for
high-risk patients (eg, those receiving chemotherapy), and for patients with
certain common health problems (eg, diabetes, chronic pain). Using current
literature and expertise, pathways identify best care. The pathway indicates
key events, such as diagnostic tests, treatments, activities, med-ications,
consultation, and education, that must occur within specified times for the
patient to achieve the desired and timely outcomes.
A case manager often
facilitates and coordinates interventions to ensure that the patient progresses
through the key events and achieves the desired outcomes. Nurses providing
direct care have an important role in the development and use of clinical
path-ways through their participation in researching the literature and then
developing, piloting, implementing, and revising clinical pathways. In
addition, nurses monitor outcome achievement and document and analyze
variances. Figure 1-2 presents an example of a clinical pathway. Other examples
of clinical pathways can be found in Appendix A.
Care mapping,
multidisciplinary action plans (MAPs), clini-cal guidelines, and algorithms are
other evidence-based practice tools that are used for interdisciplinary care
planning. These tools are used to move patients toward predetermined outcome
mark-ers using phases and stages of the disease or condition. Algorithms are
used more often in an acute situation to determine a particu-lar treatment
based on patient information or response. Care maps, clinical guidelines, and
MAPs (the most detailed of all tools) provide coordination of care and
education through hos-pitalization and after discharge (Cesta & Falter,
1999).
Because care mapping and
guidelines are used for conditions in which the patient’s progression often
defies prediction, specific time frames for achieving outcomes are excluded.
Patients with highly complex conditions or multiple underlying illnesses may
benefit more from care mapping or guidelines than from clinical pathways,
because the use of outcome markers (rather than spe-cific time frames) is more
realistic in such cases.
Through case management
and the use of clinical pathways or care mapping, patients and the care they
receive are continually assessed from preadmission to discharge—and in many
cases after discharge in the home care and community settings. These tools are
used in hospitals and alternative health care delivery systems to facilitate
the effective and efficient care of large groups of patients. The resultant
continuity of care, effective utilization of services, and cost containment are
expected to be major benefits for society and for the health care system.
Related Topics