Chapter: Medical Surgical Nursing: Management of Patients With Oncologic or Degenerative Neurologic Disorders
Degenerative Disk Disease
DEGENERATIVE DISK DISEASE
Low back pain is a
significant public health disorder in the United States (Bigos et al., 1994).
It is a challenging disorder to quantify. Current estimates are that between
22% and 65% of individuals have an episode of back pain in any given year, and
between 11% and 84% of adults have an episode within their lifetime (Walker,
2000). This results in significant economic and social costs. Acute low back
pain has a duration of less than 3 months; chronic or de-generative disease has
a duration of 3 months or longer. Most back problems are related to disk
disease.
Pathophysiology
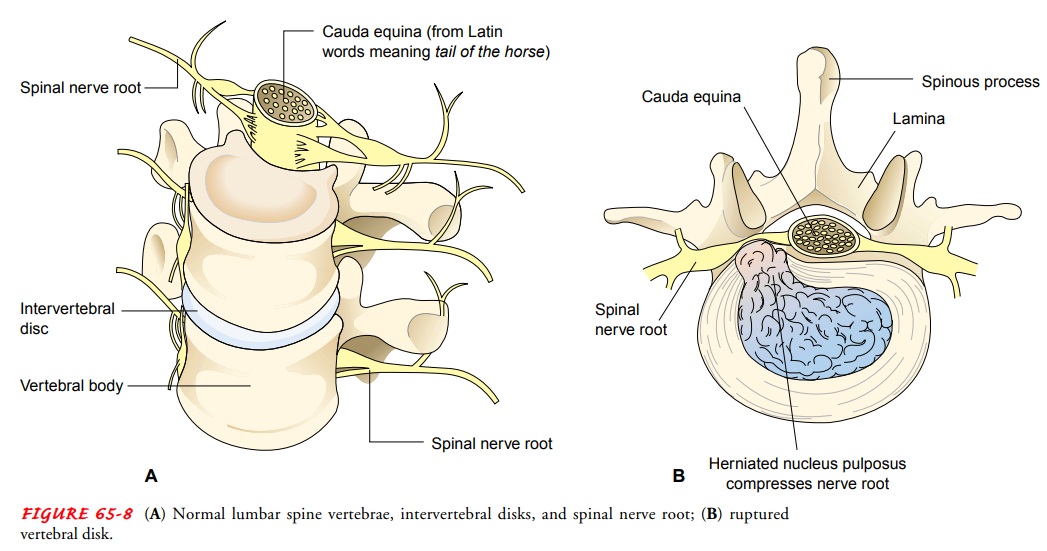
The intervertebral disk
is a cartilaginous plate that forms a cush-ion between the vertebral bodies
(Fig. 65-8A). This tough, fibrous
material is incorporated in a capsule. A ball-like cushion in the center of the
disk is called the nucleus pulposus. In herniation of the intervertebral disk
(ruptured disk), the nucleus of the disk protrudes into the annulus (the
fibrous ring around the disk), with subsequent nerve compression. Protrusion or
rupture of the nucleus pulposus usually is preceded by degenerative changes
that occur with aging. Loss of protein polysaccharides in the disk decreases
the water content of the nucleus pulposus. The devel-opment of radiating cracks
in the annulus weakens resistance to nucleus herniation. After trauma (falls
and repeated minor stresses such as lifting), the cartilage may be injured.
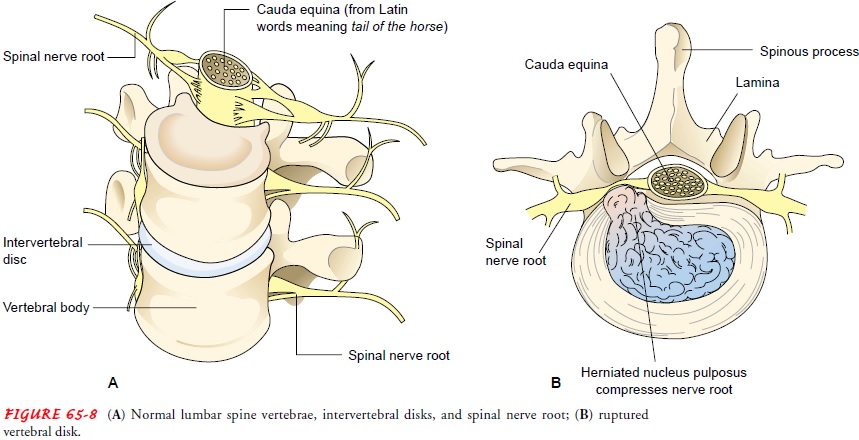
For most patients, the immediate symptoms of trauma are
short-lived, and those resulting from injury to the disk do not ap-pear for
months or years. Then, with degeneration in the disk, the capsule pushes back
into the spinal canal, or it may rupture and allow the nucleus pulposus to be
pushed back against the dural sac or against a spinal nerve as it emerges from
the spinal column (see Fig. 65-8B).
This sequence produces pain due to pressure in the area of distribution of the
involved nerve endings (radiculopathy).
Continued pressure may produce degenerative changes in the involved nerve, such
as changes in sensation and deep tendon reflexes.
Clinical Manifestations
A herniated disk with
accompanying pain may occur in any por-tion of the spine: cervical, thoracic
(rare), or lumbar. The clinical manifestations depend on the location, the rate
of development (acute or chronic), and the effect on the surrounding
structures.
Assessment and Diagnostic Findings
A thorough health history and physical examination are
impor-tant to rule out potentially serious conditions that may present as low
back pain, including fracture, tumor, infection, or cauda equina syndrome
(Bigos et al., 1994).
MRI has become the
diagnostic tool of choice for localizing even small disk protrusions,
particularly for lumbar spine disease. If the clinical symptoms are not
consistent with the pathology seen on MRI, CT and myelography are then
performed. A neu-rologic examination is carried out to determine if there is
reflex, sensory, or motor impairment from root compression and to pro-vide a
baseline for future assessment. EMG may be used to local-ize the specific spinal
nerve roots involved.
Medical Management
Herniations of the cervical and the lumbar disks occur
most com-monly and are usually managed conservatively with bed rest and
medication. The specific conservative management strategies, along with
surgical interventions for each form of herniation, are discussed next.
SURGICAL MANAGEMENT
In general, surgical
excision of a herniated disk is performed when there is evidence of a
progressing neurologic deficit (muscle weak-ness and atrophy, loss of sensory
and motor function, loss of sphincter control) and continuing pain and sciatica (leg pain re-sulting from
sciatic nerve involvement) that are unresponsive to conservative management.
The goal of surgical treatment is to re-duce the pressure on the nerve root to
relieve pain and reverse neurologic deficits (Hall, 1999). Microsurgical
techniques are making it possible to remove only the amount of tissue that is
necessary, better preserving the integrity of normal tissue and im-posing less
trauma on the body. During these procedures, spinal cord function can be
monitored electrophysiologically.
To achieve the goal of pain relief, several surgical
techniques are used, depending on the type of disk herniation, surgical
mor-bidity, and overall results of surgery:
·
Discectomy: removal of
herniated or extruded fragments of intervertebral disk
·
Laminectomy: removal of the
bone between the spinal process and facet pedicle junction to expose the neural
ele-ments in the spinal canal (Hall, 1999); allows the surgeon to inspect the
spinal canal, identify and remove pathology, and relieve compression of the
cord and roots
·
Hemilaminectomy: removal of
part of the lamina and part of the posterior arch of the vertebra
·
Partial laminectomy or
laminotomy: creation of a hole in the lamina of a vertebra (Hall, 1999)
·
Discectomy with fusion: a bone
graft (from iliac crest or bone bank) is used to fuse the vertebral spinous
process; the object of spinal fusion is to bridge over the defective disk to
stabilize the spine and reduce the rate of recurrence
·
Foraminotomy: removal of the
intervertebral foramen to in-crease the space for exit of a spinal nerve,
resulting in re-duced pain, compression, and edema
Surgical procedures for herniated cervical disk and
lumbar disk are discussed in the sections that follow.
Related Topics