Chapter: Essentials of Psychiatry: The Cultural Context of Clinical Assessment
Cultural Competence
Cultural Competence
Recent years have seen the development of
professional stand-ards for training and quality assurance in cultural
compe-tence (Lopez, 1997; Sue, 1998). This term stands for a range of
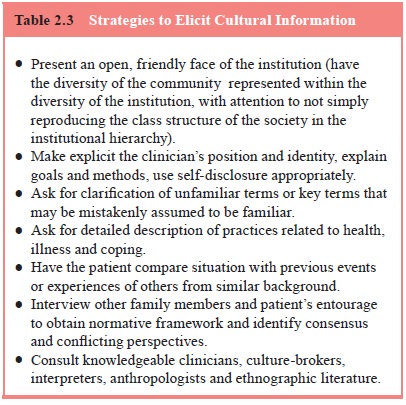
Table
2.3 Strategies to Elicit Cultural
Information
┬À
Present an open, friendly face of the institution (have the
diversity of the community represented within the diversity of the institution,
with attention to not simply reproducing the class structure of the society in
the institutional hierarchy).
┬À
Make explicit the clinicianÔÇÖs position and identity, explain
goals and methods, use self-disclosure appropriately.
┬À
Ask for clarification of unfamiliar terms or key terms that
may be mistakenly assumed to be familiar.
┬À
Ask for detailed description of practices related to health,
illness and coping.
┬À
Have the patient compare situation with previous events or
experiences of others from similar background.
┬À
Interview other family members and patientÔÇÖs entourage to
obtain normative framework and identify consensus and conflicting perspectives.
┬À
Consult knowledgeable clinicians, culture-brokers,
interpreters, anthropologists and ethnographic literature.
approaches aimed at improving the delivery of
appropriate serv-ices to a culturally diverse population. Cultural competence may
involve both culture-specific and generic strategies to address a range of
practical issues in intercultural work (Okpaku, 1998). This includes the
clinicianÔÇÖs ability to elicit cultural informa-tion during the clinical
encounter (Table 2.3), to understand how different cultural worlds of patients
and their families influence the course of the illness, and to develop a
treatment plan that empowers the patient by acknowledging cultural knowledge
and resources while allowing appropriate psychiatric intervention.
Specific cultural competence has to do with
knowledge and skills pertaining to a single cultural group, which may in-clude
history, language, etiquette, styles of child-rearing, emo-tional expression
and interpersonal interaction as well as cultural explanations of illness and
specific modalities of healing. Often, it is assumed that specific cultural
competence is assured when there is an ethnic match between clinician and
patient (e.g., aHispanic clinician treating a client from the same background).
However, ethnic matching without explicit training in models of culture and
intercultural interaction may not be sufficient to ensure that clinicians
become aware of their tacit cultural knowl-edge or biases and apply their
cultural skills in a clinically effec-tive manner.
Ethnic matching can occur at the level of the
individual, the technique, the institution, or any combination of these levels
(Weinfeld, 1999). At the level of the individual, it may be easier to establish
rapport when clinician and patient share a common background. However, there is
a risk that some issues may be left unexplored because they are taken for
granted, or are taboo and awkward to approach. There is also difficulty when
the pa-tientÔÇÖs expectations of a fellow community member are not met because
the clinician applies the rules and limits dictated by pro-fessional training.
This may include expectations of receiving special treatment, of being cured
quickly, of becoming friends, or intervening inappropriately on behalf of other
family or com-munity members.
In many cases, however, ethnic matching is only
crude or approximate. For example, the term Hispanic covers a broad ter-ritory with many cultural, educational
and social class differences that transcend language. Indeed, there is enormous
intracultural variation and no one person carries comprehensive knowledge of
his or her own cultural background, so there is always the need to explore
local meanings with patients.
In the course of professional training, clinicians
may dis-tance themselves from their own culture of origin and become reluctant
or unable to use (or understand the impact of) their tacit cultural knowledge
in their clinical work. Clinicians from ethnic minority backgrounds may resent
being pigeon-holed and expected to work predominately with a specific
ethnocultural group. Patients may have complex reactions to meeting a
clini-cian from the same background. These issues require attention and
sensitive exploration just as much as the feelings evoked by meeting someone
from a different background.
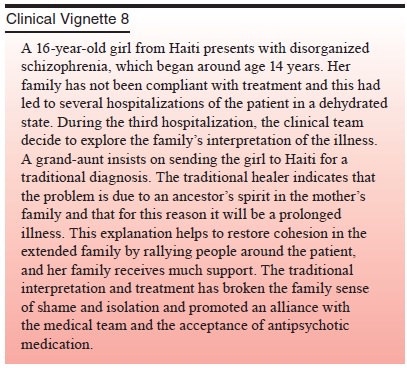
At the level of technique, the clinician familiar
with a spe-cific ethnocultural group learns to modify his or her approach to
take advantage of culturally supported coping strategies. For example, religious
practices, family and community supports, and appeals to specific cultural
values may all provide useful strategies for symptom management and improved
functioning. Traditional diagnostic and treatment methods may be used in
concert with conventional psychiatric treatments. The clinician may use his or
her own person differently in recognition of cul-tural notions of healing
relationships, adopting a more authorita-tive stance, making selective use
self-disclosure, or participating in symbolic social exchanges with patients
and their extended families to establish trust and credibility.
At the level of institutions, ethnic match is
represented in the organization of the clinical service, which should reflect
the composition of the communities it serves (Kareem and Littlewood, 1992).
This is not merely a matter of hiring prac-tices but also involves creating
structures that allow a measure of community feedback and control of the
service institution. When people feel a sense of ownership in an institution,
they will evince a higher level of trust and utilization. It is important,
therefore, for clinicians to understand how the institutional set-ting in which
they are working is seen by specific ethnocultural communities.
Increasingly, clinicians work in settings where
there is great cultural diversity that precludes reaching a high level of
specific competence for any one group. Changes in migration patterns and new
waves of immigrants and refugees lead to cor-responding changes in patient
populations. For all of these rea-sons, it is crucial to supplement specific
cultural competence with more generic competence that is based on a broad
theoreti-cal understanding of culture and ethnicity. Generic cultural
com-petence abstracts general principles from specific examples of cultural
differences. The core of generic competence resides in cliniciansÔÇÖ
understanding of their own cultural background and assumptions, some of which
are related to ethnicity and religion and many of which derive from
professional training and the con-text of practice. Appreciating the wide range
of cultural variation in gender roles, family structures, developmental
trajectories, explanations of health and illness, and responses to adversity
allows the clinician to ask appropriate questions about areas that would
otherwise be taken for granted. The culturally competent clinician has a keen
sense of what he or she does not know and a solid respect for difference. While
empathy and respectful in-terest allow the clinician gradually to come to know
anotherÔÇÖs world, the clinician must tolerate the ambiguity and uncertainty that
comes with not knowing. In the end, patients are the experts on their own
experiential worlds and cultural context must be reconstructed simultaneously
from the inside out (through the patientÔÇÖs experience) and from the outside in
(through an appre-ciation of the social matrix in which the patient is
embedded).
The wide range of specific and generic skills
needed for competent intercultural work means that most clinicians will find it
helpful to work in multidisciplinary teams that contain cultural diversity that
reflects the patient population. A variety of models for such teamwork have
been developed (Kareem and Littlewood, 1992; Kirmayer et al., 2003).
Related Topics