Chapter: Essentials of Psychiatry: Listening to the Patient
Crucial Attitudes that Enable Effective Listening
Crucial
Attitudes that Enable Effective Listening
The first step in developing good listening skills
involves coming to grips with the importance of inner experience in psychiatric
treatment and diagnosis. The Diagnostic
and Statistical Man-ual of Mental Disorders, Fourth Edition (American
Psychiatric Association, 1994) and International Classifi cation of Diseases, 10th Revision (World
Health Organization, 1992) have been enor-mous advances in reliability and
accuracy of diagnosis, but their emphasis on seemingly observable phenomena has
allowed the willing user to forget the importance of inner experience even in
such basic diagnoses as major depressive disorder. Consider the symptom
“depressed mood most of the day” or “markedly dimin-ished interest or pleasure”
or even “decrease or increase in appe-tite”. These are entirely subjective
symptoms. Simply reporting depression is usually not sufficient to convince a
psychiatrist that a diagnosis of depression is warranted. In fact, the vast
majority of psychiatric patients are so demoralized by their illnesses that
they often announce depression as their first complaint. Further, there are a
significant number of patients who do not acknowl-edge depression yet are so
diagnosed. The clinician might well comment, “Sitting with him makes me feel
very sad”.
The psychiatrist must listen to much more than the
pa-tient’s overt behavior. There are qualities in the communica-tion, including
the inner experiences induced in the listener, that should be attended to. The
experienced clinician listens to the words, watches the behavior, engages in
and notices the ongo-ing interaction, allows himself/herself to experience
his/her own inner reactions to the process, and never forgets that depression and
almost all other psychiatric symptoms are exclusively pri-vate experiences.
The behavior and interactions are useful inso-far as they assist the
psychiatrist in inferring the patient’s inner experience.
Therefore, to convince a clinician that a patient
is de-pressed, not only must the patient say she/he is depressed, but the observable
behavior must convey it (sad-looking face, sighing, unexpressive intonations,
etc.); the interaction with the inter-viewer must convey depressive qualities
(sense of neediness, sad-ness induced in the interviewer, beseeching qualities
expressed, etc.). In the absence of both of these, other diagnoses should be
considered, but in the presence of such qualities, depression needs to remain
in the differential diagnosis.
Even when we make statements about brain function
with regard to a particular patient, we use this kind of listen-ing, generally,
by making at least two inferences. We first listen to and observe the patient
and then infer some aspect of the pa-tient’s private experience. Then, if we
possess sufficient scien-tific knowledge, we make a second inference to a
disturbance in neurochemistry, neurophysiology, or neuroanatomy. When
psychiatrists prescribe antidepressant medication, they have in-ferred from
words, moved into inner experiences, and come to a conclusion that there is
likely a dysregulation of serotonin or norepinephrine in the patient’s brain.
As one moves towards treatment from diagnosis, the
con-tent of inner experience inferred may change to more varied states of
feelings, needs, and conflicts, but the fundamental process of listening
remains the same. The psychiatrist listens for the mean-ing of all behavior, to
the ongoing interpersonal relationship the patient attempts to establish, and
to inner experiences as well.
Despite all of the technological advances in
medicine in general and their growing presence in psychiatry, securing or
eliciting a history remains the first and central skill for all physi-cians.
Even in the most basic of medical situations, the patient is trying to
communicate a set of private experiences (how does one describe the qualities
of pain or discomfort?) that the physician may infer and sort into possible
syndromes and diagnoses. In psychiatry, this process is multiplied, as
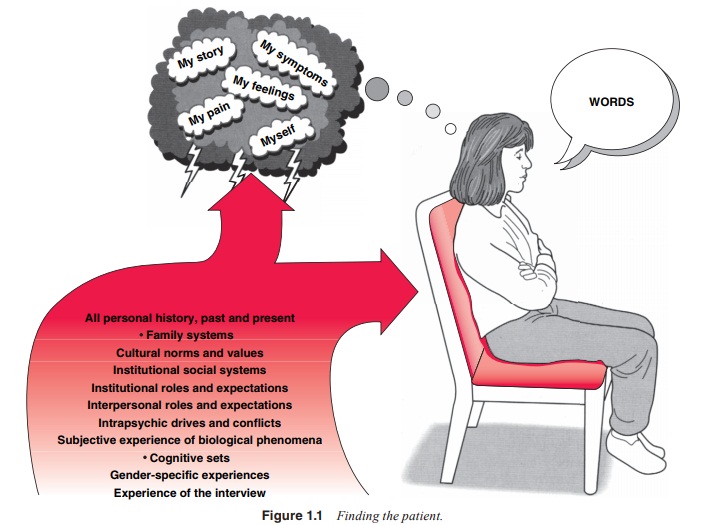
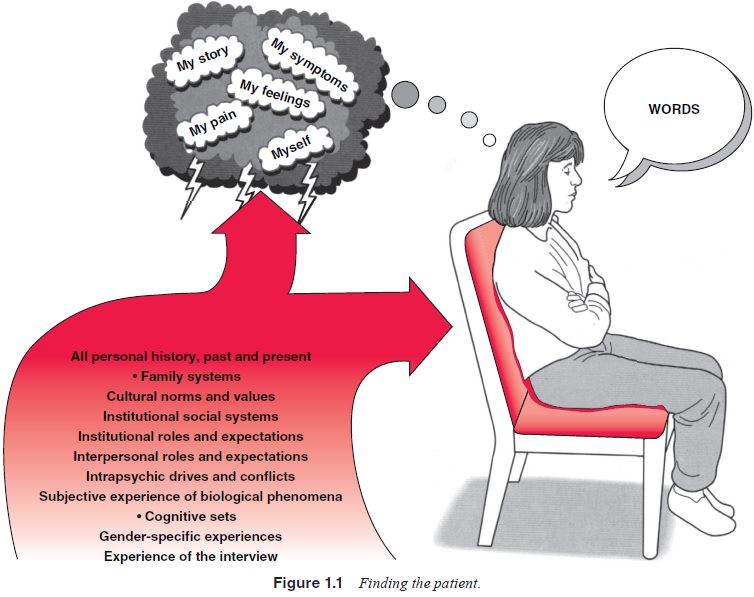
indicated in Figure 1.1. William Styron (1990), a prizewinning novelist, had to
go to ex-traordinary lengths in his eloquent attempt to convey the “searing
internal mental pain” that he experienced when suffering from a major
depression.
The qualitative aspects of private experience
remain, to this day, a major problem in philosophy. It was the basis of Rene
Descartes’ (1991) philosophical doubting that became the fun-damental
intellectual underpinning of Western thought for so long. Edmund Husserl (1977)
used it as the basis for an entire philosophical system, phenomenology, which was
a forerunner of existentialism, which was so influential in both American and
European psychiatry in the 1950s and 1960s (May et al., 1958; Binswanger, 1963).
Silvano Arieti (1967) hypothesized that cognitive
devel-opment produces changes over time in the inner experience of various
affects. Does a person with borderline personality disor-der experience
“anxiety” in the same qualitative and quantitative manner in which a neurotic
person does? What is the relationship between sadness and guilt and the empty
experiences of depres-sion? This perspective underlies the principle
articulated in text after text on interviewing that emphasizes the importance
of es-tablishing rapport in the process of history taking. It is incredibly
easy for the psychiatrist to attribute to the patient what she/he would have
meant and what most people might have meant in using a particular word or
phrase. The sense in the narrator that the listener is truly present,
connected, and with the patient enor-mously enhances the accuracy of the story
reported.
Words that have been used to describe this process
of constant attention to and inference of inner experience by the listener
include interest, empathy (Rogers, 1951; Kohut, 1991; Truax, 1963),
attentiveness and noncontingent positive regard (Truax, 1963). However, these
are words that may say less than they seem to. It is the constant curious
awareness on the listener’s part, that she/he is trying to grasp the private
inner experience of the patient, and the storyteller’s sense of this stance by
the psy-chiatrist that impels the ever more revealing process of history
taking. This quality of listening produces what we call rapport, without which
psychiatric histories become spotty, superficial and even suspect. There are no
bad historians, only patients who have not yet found the right listener.
In treatment, we even find empirical data to
support this perspective. The two most powerful predictors of outcome in any
form of psychotherapy are empathy and the therapeutic al-liance (Horvath and
Luborsky, 1993; Greenson, 1978). This has been shown again and again in study
after study for dynamic therapy, cognitive therapy, behavior therapy and even
medica-tion management (Elkin et al.,
1989). This led some researchers and theorists to propose that the power of
psychotherapy can be understood solely as a remoralization phenomenon based on
sup-port and empathy (Frank, 1973; Omer and London, 1989). The truth of this
can be seen in the remarkable therapeutic success of the “clinical management”
cell of the National Institutes of Mental Health Collaborative Study on the
Treatment of Major Depression. Although the Clinical Management Cell was not as
effective as the cells that included specific drugs or specific
psychotherapeutic interventions, 35% of patients with moder-ate to severe major
depressive disorder improved significantly with carefully structured supportive
clinical management alone (Elkin et al.,
1989).
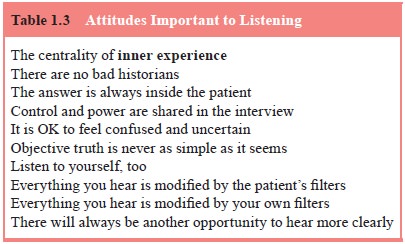
Helpful psychiatric listening requires a
complicated atti-tude toward control and power in the interview (see Table
1.3). The psychiatrist invites the patient/storyteller to collaborate as an
active informer. He is invited, too, to question and observe him-self. This
method of history taking remains the principal tool of general clinical
medicine. However, as Freud pointed out, these methods of active uncovering are
more complex in the psychic
realm. The use of the patient as a voluntary
reporter requires that the investigator keep in mind the unconscious and its
power over the patient and listener. Can the patient be a reliable objective
wit-ness of himself or his symptoms? Can the listener hold in mind his own set
of filters, meanings, and distortions as he hears? The listener translates for
himself and his patient the patient’s articu-lation of his experience of
himself and his inner world into our definition of symptoms, syndromes, and
differential diagnoses which make-up the concept of the medical model.
Objective–descriptive examiners are like detectives
clos-ing in on disease. The psychiatric detective enters the inquiry with an
attitude of unknowing and suspends prior opinion. The techniques of listening
invoke a wondering and a wandering with the patient. Periods of head scratching
and exclamations of “I’m confused”, or “I don’t understand”, or “That’s awful!”
or “Tell me more”, allow the listener to follow or to point the way for the
dyad. Finally, clear and precise descriptions are held up for scrutiny, with
the hope that a diagnostic label or new information about the patient’s
suffering and emotional pain is revealed.
It is embarking on the history taking journey
together – free of judgments, opinions, criticism, or preconceived notions –
that underpins rapport. Good listening requires a complex understanding of what
objective truth is and how it may be found. The effective psychiatrist must
eschew the traditional medical role in interviewing and tolerate a
collaborative, at times me-andering, direction in which control is at best
shared and some-times wholly with the patient. The psychiatrist constantly
asks: What is being said? Why is it being said at this moment? What is the
meaning of what is being said? In what context is all this emerging? What does
that tell me about the meaning and what does it reflect about the
doctor–patient relationship?
Related Topics