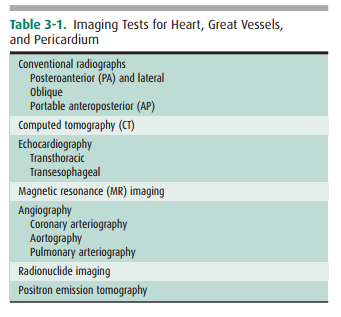
Chapter: Basic Radiology : Imaging of the Heart and Great Vessels
Conventional Radiographs
TECHNIQUES AND
NORMAL ANATOMY
A variety of techniques have been
developed to evaluate the heart and great vessels (Table 3-1). In this section,
we briefly describe the major tests used in imaging this system.
Conventional
Radiographs
The most common imaging test for
evaluating the heart and great vessels is the chest radiograph, which consists
of an up-right posterior-to-anterior (PA) and left lateral (LAT) pro-jections.
The terms PA and left lateral refer to the direction the x-ray beam takes through
the body before it reaches the radiographic cassette. Chest radiographs are
usually obtained with high kilovoltage and milliamperage to minimize expo-sure
time and cardiac motion. When possible, the distance between the x-ray tube
source and the film is at least 6 feet to minimize magnification and
distortion.
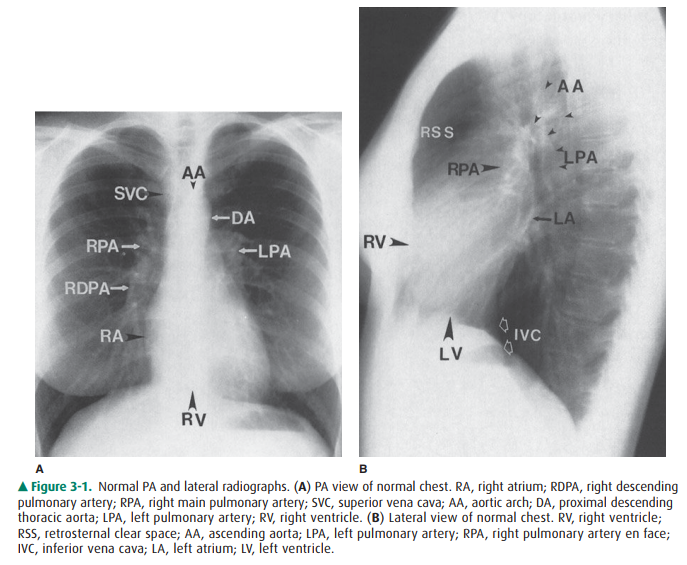
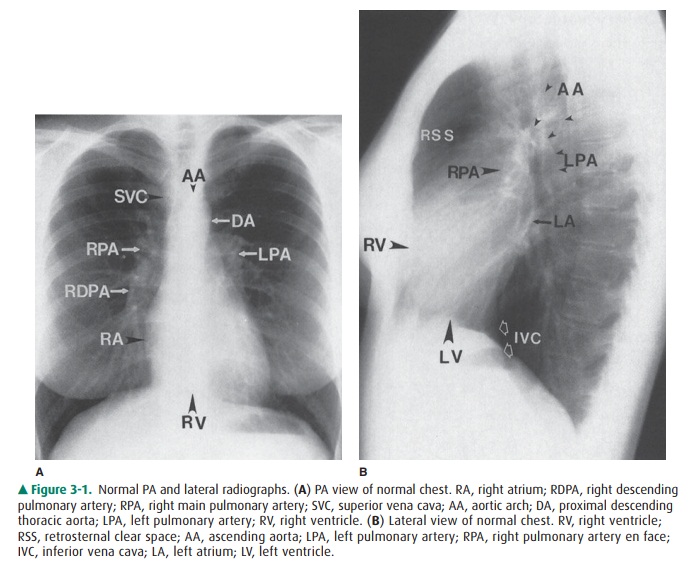
The examination is ideally
performed with the patient at maximal inspiration. A good rule of thumb for
estimating adequate inspiration is to be able to count 9 to 10 posterior ribs
or 5 to 6 anterior ribs from the lung apices to the hemidi-aphragms through the
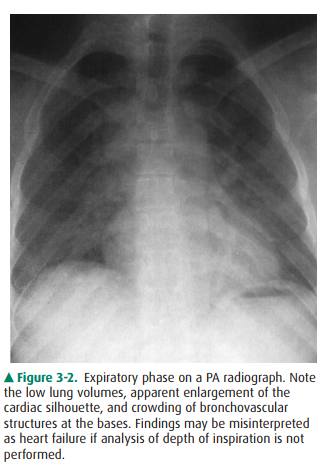
aerated lungs (Figure 3-1). When a chest radiograph is taken in the expiratory
phase of respira-tion, the patient may appear to have cardiomegaly, vascular
congestion, and even pulmonary edema. This appearance, however, is merely
artifactual and caused by the lack of inspi-ration (Figure 3-2).
Severely ill, debilitated
patients or patients who cannot be transported to the radiology department can
have their chest radiographs obtained with a portable x-ray machine. Patients
in the ICU who have intravascular catheters or who are undergoing mechanical
ventilation frequently have chest radiographs performed as a survey for
compli-cations that may not be revealed by physical examination or laboratory
data. These examinations are done with the cassette placed behind the patient
in bed and are therefore anterior-to-posterior (AP) projections. The technical
fac-tors, which are controlled by the technologist at the time of the
examination, vary with the size of the patient and the distance of the
radiographic plate from the x-ray source (or machine). An attempt is still made
to obtain the examina-tion during maximum inspiration, but this objective may
be difficult to achieve in some patients, especially those who have dyspnea.
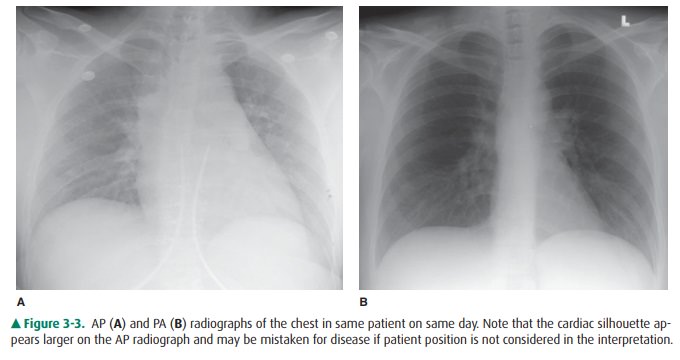
With the patient in the supine
position, there is normally a redistribution of blood flow to the upper lobe
pulmonary veins (cephalization), and the heart may appear enlarged rela-tive to
its appearance on the upright PA radiograph, because of magnification (Figure
3-3). Some patients are able to sit for their examinations, whereas others are
radiographed in a semiupright position. Ideally, the technologist should mark
the exact position of the patient when the radiograph is ob-tained, and the
date and time of the examination should be recorded in all cases. Changes in patient
positioning and ven-tilator settings can have substantial effects on the
radiographic appearance and must be taken into account when evaluating any
change in the radiograph from a previous study.
The chest radiograph, whether it
is obtained in the up-right, semiupright, sitting, or supine position, should
almost always be the initial screening examination in the evaluation of the
cardiovascular system. Because it is essentially a screening study, the chest
x-ray must be correlated with the clinical symptoms and physical examination to
determine the overall significance of the radiographic findings. This
in-formation is also used to decide if other imaging tests are ap-propriate and
which ones will potentially result in the highest diagnostic yield. Decisions
regarding further imaging also depend on the impact on the clinical management
of the pa-tient, the potential for treatment of any abnormality that may be
discovered, the cost and availability of the technique, and the expertise of
the interpreting radiologist.
The conventional radiograph is an
excellent screening test for the patient suspected of having disease involving
the heart and great vessels, because the overall anatomy of these areas is
demonstrated well. Whenever possible, all radiographs should be reviewed with
all prior relevant imaging studies. Even when a prior chest radiograph is not
available, additional in-formation may be ascertained by reviewing other prior
im-ages such as thoracic spine or rib-detail image when available. Advanced
imaging studies such as computed tomography (CT) and magnetic resonance (MR)
imaging can also be used to help clarify complex findings on chest radiographs.
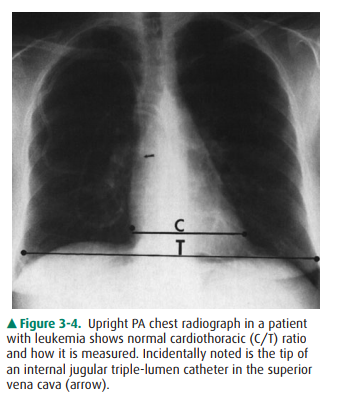
The normal cardiac silhouette
size may be determined by the cardiothoracic ratio, a measurement obtained from
the PA view. This ratio is calculated by dividing the transverse cardiac
diameter (measured from each side) by the widest di-ameter of the chest
(measured from the inner aspect of the right and left lungs near the
diaphragm). The average normal value for this ratio in adults is 0.50, although
up to 60% may be normal (Figure 3-4). A measurement over 50% is gener-ally
considered abnormal in an upright inspiratory-phase PA film, although this may
not always be clinically significant. The cardiothoracic ratio cannot be
reliably used for the AP projection of the chest, because the heart is
magnified (see Figure 3-3). The size of the patient and the degree of lung
ex-pansion also should be considered. For instance, in a small person with a
petite frame and a small thoracic cage, the heart size may be normal, but the
cardiothoracic ratio may measure over 50%. Similarly, if the patient has
pulmonary disease such as emphysema, the heart may be enlarged, but because of
the overinflation of the lungs, the cardiothoracic ratio may still be normal.
In clinical practice, most radiolo-gists do not perform this measurement and
rely on experi-ence and “gestalt” to evaluate heart size.
The contours of the heart,
mediastinum, and great ves-sels on the PA view should be evaluated on each
chest film (see Figure 3-1A). A reasonable approach is to begin in the upper
right side of the mediastinum just lateral to the spine and below the right
clavicle. The curved soft-tissue shadow represents the right border of the
superior vena cava (SVC). The border of the SVC forms an interface with the
lung and should not be confused with the right paratracheal stripe. Below the
SVC is the right cardiac border formed by the right atrium. The inferior heart
border, or base of the heart, is the area just above the diaphragm and is
composed pri-marily of the right ventricle, although there is some
contri-bution from the left ventricular shadow. The left ventricle makes up the
majority of the apex of the heart, which points to the left of the spine. The
origins of the right and left pulmonary arteries are generally well demarcated
on the normal PA film as they emerge from the mediastinum. The most prominent
and recognizable component of the right pulmonary artery, the right descending
pulmonary artery (RDPA), is seen just to the right of the superior cardiac
bor-der and descends inferiorly. It can usually be easily followed until it
branches. The left main pulmonary artery is less well defined, but its origin
can usually be seen above and lateral to the left atrial appendage just before
it branches. When en-larged, the main pulmonary artery may be seen superimposed
over the left pulmonary artery and filling in the normal spacebetween the left
pulmonary artery and transverse aortic arch (the AP window). The aorta
originates posterior and to the right of the main pulmonary artery, and the
border of the as-cending portion of the aorta can usually be seen superim-posed
on the inferior portion of the SVC. The majority of the transverse arch is not
outlined by air and therefore cannot be seen as it crosses the mediastinum.
However, the distal trans-verse and descending aorta can be seen to the left of
the mediastinum as it turns inferiorly. The left border of the descending
thoracic aorta should be followed down to the aor-tic hiatus. Any loss of this
contour or any contour abnormality may indicate pathology and should be
investigated. Dilation or ectasia, localized bulges, and calcification may
occur within the aorta as a normal part of the aging process, but should be
viewed as abnormal in younger individuals. Of course, the spine, ribs, adjacent
soft tissues, and upper ab-dominal contents should all be scrutinized. The left
atrium lies just inferior to the tracheal carina, but it is usually not
visualized as a discrete structure on the normal PA view.
The lateral view of the chest
also reveals important infor-mation regarding the cardiac contour (see Figure
3-1B). Just behind the sternum there is normally a radiolucent area called the
retrosternal clear space (RSS). This region repre-sents lung interposed between
the chest wall and the anterior margin of the ascending aorta. Any density
present within the RSS may be due to an anterior mediastinal mass or
post-surgical changes. The anterior border of the cardiac shadow is composed
primarily of the anterior wall of the right ventri-cle. Right ventricular
enlargement may also encroach into the retrosternal clear space. The posterior
margin of the cardiac silhouette is formed by the left atrium and left
ventricle. Just posterior and inferior to the left ventricle is a linear
soft-tissue shadow leading into the heart formed by the inferior vena cava
(IVC). The left ventricular shadow should not project more than 2 cm posterior
to the posterior border of the IVC. The transverse aortic arch can usually be
discerned on the normal lateral chest film as a smooth curving shadow
origi-nating anteriorly, crossing the mediastinum in a semilunar fashion, and
then descending posteriorly as a linear shadow superimposed over the vertebral
bodies. The left pulmonary artery (LPA) produces a similar curvilinear shadow
just below the aortic arch before it branches. Just below the LPA, the left
main/left upper lobe bronchus can be seen (projected end-on) as a round
lucency. The right pulmonary artery (RPA) is seen en face down its lumen as an
oval soft-tissue structure anterior to the bronchus intermedius and below and
anterior to the left pulmonary artery.
Related Topics