Chapter: Medical Surgical Nursing: Assessment and Management of Female Physiologic Processes
Contraception - Management of Normal and Altered Female Reproductive Function
CONTRACEPTION
Each
year, more than half of the pregnancies in the United States are unintended
(Centers for Disease Control and Prevention, 1999). Although unintended
pregnancies occur in women of all ages, incomes, and racial and ethnic groups,
the highest rates occur among adolescents, lower-income women, and
African-American women (U.S. Surgeon General, 2001). Adolescents are more
likely to experience pregnancy complications and are more prone to have
low-birthweight babies. Teen mothers are less likely to obtain a high school
diploma and are more likely to live in poverty. Of women undergoing abortions,
many did not use contraception in the month they became pregnant, while others
never use any method. It seems that women often fail to use ef-fective methods
consistently or at all. Nurses can assist with in-formation and support. Women
sometimes fear that they will get cancer and fear other risks from
contraception. Women often re-port using their contraceptive method
inconsistently, which makes all methods less effective.
Many
women who are sexually active or who are considering becoming sexually active
can benefit from learning about contra-ception. Fewer unwanted pregnancies may
reduce the number of abortions, abused children, stressed families, and infant
mortal-ity and morbidity. It is important that women receive unbiased and
nonjudgmental information, understand the benefits and risks of each method,
learn about alternatives and how to use them, and receive positive
reinforcement and acceptance of their choice.
Nurses
involved in helping patients make contraceptive choices need to listen,
educate, spend time answering questions, and assist patients in choosing the
method they prefer. Methods and prac-tices to prevent unwanted or unplanned
pregnancies and births.
Abstinence
Abstinence,
or celibacy, is the only completely effective means of preventing pregnancy.
Abstinence may not be a desired or avail-able option for many women because of
cultural expectations and their own and their partner’s values and sexual needs
Sterilization
After
abstinence, sterilization by bilateral tubal occlusion or va-sectomy is the
most effective means of contraception. Both pro-cedures must be considered
permanent because neither is easily reversible. Women and men who choose these
methods should be certain that they have completed their childbearing, no
mat-ter how the circumstances in their life may change. Often, deci-sions are
made that may be regretted later. Some gynecologists suggest a waiting period
to ensure that the patient is certain about a potentially irreversible
decision.
TUBAL LIGATION
Female
sterilization by tubal ligation is one of the most common operations performed
on women. More than 600,000 tubal li-gations are performed in the United States
every year ( Jamieson, Hillis, Duerr et al., 2000). Tubal ligation is usually
performed as a same-day surgical procedure. The procedure is carried out by
la-paroscopy, with the patient receiving a general or local anesthetic. The
laparoscope, a small periscope-like optical instrument, is in-serted through a
small umbilical incision. Carbon dioxide is in-troduced to lift other abdominal
organs away from the tubal area. The fallopian tubes are visualized and may be
coagulated, sutured (Pomeroy procedure), or ligated with a rubber band or a
spring clip, thereby disrupting their patency. Many sterilizations are
per-formed with bipolar coagulation. Silicone bands and spring clips are also
being used. Spring clips have the highest rate of pregnancy following
sterilization. A new procedure, selective tubal occlusion procedure, uses a
0.6-inch metal coil or spring that is inserted into the fallopian tubes through
the cervix, thus avoiding the need for laparoscopy or a surgical incision
(Association of Reproductive Health Professionals, 2002). This method works by
inducing ob-struction of the tubes by scar tissue.
Despite
a very high rate of effectiveness, any woman who has undergone tubal ligation
but misses a period should be tested for pregnancy because ectopic and
intrauterine pregnancies, although rare, may occur. Ovulation and menstruation
are not affected by sterilization, although some women report heavier menstrual
bleeding and more cramping after tubal ligation. Vasectomy and laparoscopic
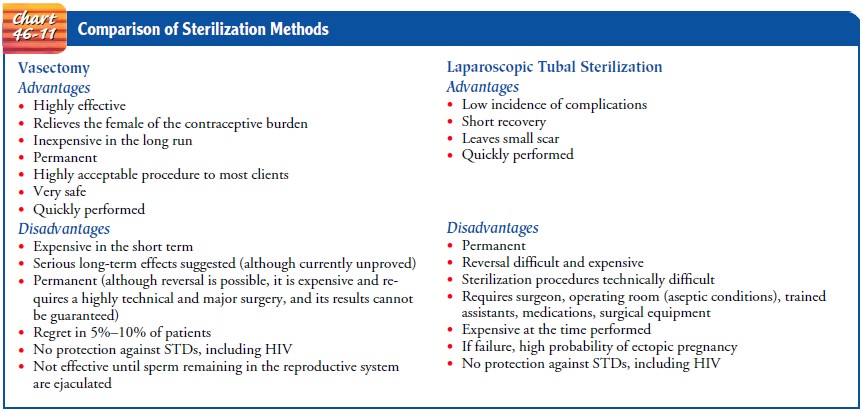
tubal ligation are compared in Chart 46-11.
Before
undergoing tubal ligation, the patient should be in-formed that an IUD, if
present, will be removed. If the patient is taking oral contraceptives, she
usually continues them up to the time of the procedure. Postoperatively, women
may experience abdominal or shoulder discomfort for a few days, related to the
carbon dioxide gas and the manipulation of organs. The woman is instructed to
report heavy bleeding, fever, or pain that persists or increases. The patient
should avoid intercourse, strenuous ex-ercise, and lifting for 2 weeks. Risks
of the procedure are minimal and are more often related to the anesthesia than
to the surgery itself. Risk is increased in women with diabetes, previous
ab-dominal or pelvic surgery, or obesity.
Oral Contraceptives
Oral
contraceptive preparations of synthetic estrogen (estradiol) and progesterone
(desogestrel, ethynodiol diacetate, lev-onorgestrel, norethindrone, norethindrone
acetate or norgestrel) are currently used by many women. They block ovarian
stimula-tion by preventing the release of FSH from the anterior pituitary
gland. In the absence of FSH, a follicle does not ripen, and ovu-lation does
not occur. This is the mechanism of action of oral contraceptives. Progestins
(synthetic forms of progesterone) sup-press the LH surge, prevent ovulation,
and also render the cervi-cal mucus impenetrable to sperm. Synthetic estrogens
and progestin, found in the many oral contraceptive variations avail-able,
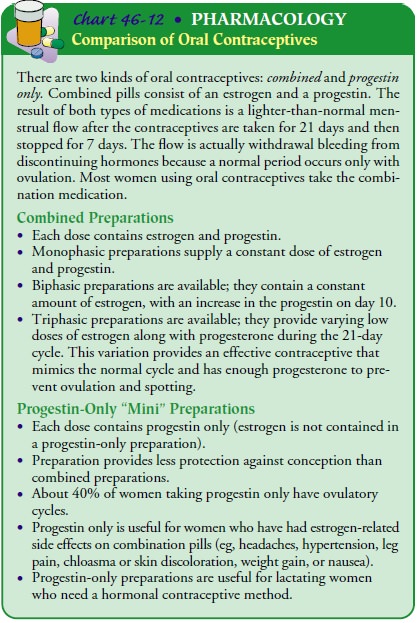
differ in androgenic activity (Chart 46-12).
BENEFITS AND RISKS
In general, no definite long-term undesirable effects have been ob-served with prolonged oral contraceptive use. Resumption of normal menses is delayed 2 to 3 months in about 20% of oral con-traceptive users. Venous thromboembolism has occurred with use of oral contraceptives, but it occurs less now than years ago, when estrogen concentrations in oral contraceptives were higher. Ve-nous thromboembolism is less than half as likely to occur with oral contraceptives than with pregnancy. Desogestrel, a new progestin, may be slightly more likely to be associated with venous throm-boembolism, but the risk is still very low.
Gallbladder problems (eg, cholestasis) may occur. Fetal
anomalies do not appear to be a concern, and normal reproductive tract function
and fertility are restored after oral contraceptive use is discontinued.
However, most health care providers recommend that women use a barrier
contraceptive method for 1 to 2 months after stopping the pill before becoming
pregnant so that the accurate date of the last menstrual period is available to
date the pregnancy.
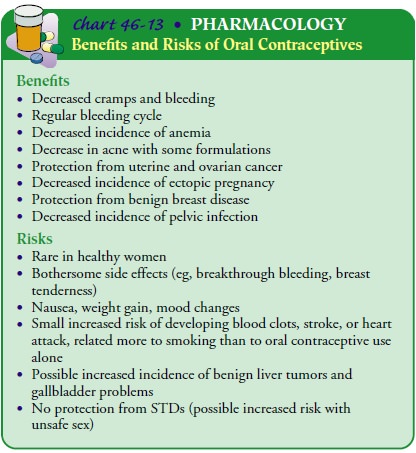
Some
of the benefits of using oral contraceptives include a re-duction in the
incidence of benign breast disease, improvement in acne, reduced risk of
uterine and ovarian cancers, anemia, and pelvic infection.
A few
patients experience adverse reactions when using oral contraceptives. These
include nausea, depression, headache, weight gain, leg cramps, and breast
soreness. Usually, these symp-toms subside after 3 or 4 months. Because such
symptoms are sometimes related to sodium and water retention caused by
es-trogen, a smaller dose of the hormone or a different hormonal combination
may alleviate the problem. Many patients experience spotting in the first month
taking the pill or if they take it irregularly, so they need to be reassured
and advised to take a pill every 24 hours, as prescribed. Chart 46-13 describes
the benefits and risks of oral contraceptive use.
CONTRAINDICATIONS
Absolute
contraindications include current or past thromboem-bolic disorder,
cerebrovascular disease, or artery disease; known or suspected breast cancer;
known or suspected current or past estrogen-dependent neoplasia; pregnancy;
current or past benign or malignant liver tumor; impaired liver function;
congenital hy-perlipidemia; and undiagnosed abnormal vaginal bleeding.
Relative
contraindications include hypertension, bile-induced jaundice, acute phase of
mononucleosis, and sickle cell disease. Women older than 35 who smoke are at
risk for cardiac problems and should not use oral contraceptives. Occasionally,
neuro-ocular complications arise, but a cause-and-effect relationship has not
been established. If visual disturbances occur, oral contra-ceptives should be
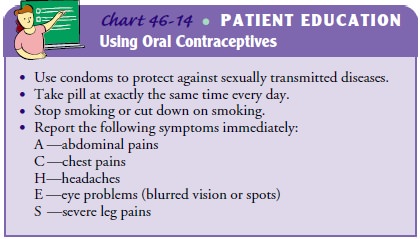
discontinued (Chart 46-14).
Some
gynecologists allow patients with migraine headaches to take oral
contraceptives if the headaches do not worsen with use or so long as the patient
has no neurologic symptoms. (A young woman who has blurred vision with a
migraine will probably be discouraged from taking oral contraceptives.)
Diabetes is also prob-lematic, although some diabetes specialists allow their
patients to use oral contraceptives with careful glucose monitoring.
Leiomy-omas (fibroid tumors) of the uterus can enlarge with oral contra-ceptive
use. Patients with this condition are advised and monitored carefully; if
fibroids enlarge, they are advised to discontinue oral contraceptives and
choose another contraceptive method.
Injectable Contraceptives
DEPO-PROVERA
An intramuscular injection of Depo-Provera, a long-acting prog-estin, every 3 months inhibits ovulation and provides a reliable and
convenient contraceptive method. It can be used by lactat-ing women and those
with hypertension, liver disease, migraine headaches, heart disease, and
hemoglobinopathies. Women who use this method must be prepared for irregular or
no bleeding. With continued use, irregular bleeding episodes and spotting
de-crease, and amenorrhea usually occurs.
Advantages
include reduction of menorrhagia, dysmenorrhea, and anemia. It may reduce the
risk of pelvic infection and has been associated with improvement in
hematologic status in women with anemia due to heavy menstrual bleeding and
women with sickle cell disease; it has also been associated with a reduced
frequency of seizures in women with seizure disorders. It also reduces the risk
of endometrial cancer (ACOG Technical Bulletin #198,
1995).
Potential
disadvantages include irregular menstrual bleeding, bloating, headaches, hair
loss, decreased sex drive, and weight loss or weight gain. Fertility may be
delayed when women discon-tinue this method; therefore, other methods of contraception
may be more appropriate for the woman who wishes to conceive within a year of
discontinuing contraception.
Depo-Provera
is contraindicated in women who are pregnant and those who have abnormal
vaginal bleeding of unknown cause, breast or pelvic cancer, or sensitivity to
synthetic progestin. The long-term effects on the infant of a nursing mother
who uses Depo-Provera are unknown but are thought to be negligible.
Depo-Provera does not protect against STDs. Bone density is temporarily
decreased while using this method, but this does not seem to be a long-term
health risk.
LUNELLE
Lunelle,
a contraceptive that is a combination of medroxyprog-esterone (progestin) and
estradiol (estrogen), has been shown to be very effective at preventing
pregnancy in clinical trials. An in-tramuscular injection is administered every
28 to 30 days. It pro-vides immediate efficacy if given within the first 5 days
following the start of a normal menstrual period. Return to ovulation oc-curs
more quickly than with Depo-Provera, usually within 2 to 4 months. The
contraindications and cautions are the same as those for oral contraceptives.
Effectiveness depends on the woman’s compliance with the regimen. Similar to
other nonbarrier con-traceptive methods, Lunelle does not protect against HIV
infection or other STDs. Light, regular monthly bleeding occurs.
Implant Contraceptive
The
Norplant system is a reversible, low-dose, progestin-only contraceptive device
consisting of several soft Silastic capsules or implants that are inserted
under the skin of the woman’s upper arm. The implant releases the progestin
levonorgestrel over 5 years, thereby inhibiting ovulation. While still
FDA-approved, it is anticipated that Norplant will not be available in the
future. However, additional implant contraceptives are expected to be-come
available in the near future. Contraindications to using these systems are
acute liver disease or liver tumors, pregnancy, unexplained vaginal bleeding,
breast cancer, and a history of thrombophlebitis or pulmonary embolism.
Common
side effects include irregular bleeding, weight gain, acne, and hair growth or
hair loss. If patients are aware of these dis-advantages and side effects, they
are more likely to tolerate the im-plant and continue using it. The patient
should report headaches or visual symptoms to a health care provider because
rare instances of idiopathic intracranial hypertension have been associated
with the implant. Papilledema must be ruled out if headaches occur.
Insertion,
minor surgery that is relatively painless, is per-formed under aseptic
conditions in an outpatient setting such as an office or clinic. A small
incision is made in the inner upper arm after the patient receives a local
anesthetic. The capsule or cap-sules are inserted within the first 7 days of
the menstrual cycle to avoid the possibility of a preexisting pregnancy. The
contracep-tive effect occurs within 24 hours and lasts for 5 years. Insertion
usually takes about 15 minutes. Although the implants can be re-moved at any time,
it can be a more difficult and lengthy proce-dure because over time tissue
encapsulates the implants. Women who have regular bleeding with an implant
method are at higher risk for pregnancy and should be counseled to have a
pregnancy test if the regular bleeding stops.
New Hormonal Methods of Contraception
Two
new hormonal methods of contraception are Ortho Evra and NuvaRing. Ortho Evra
is a thin, beige, matchbook-sized square that releases an estrogen and a
progestin continuously. It is changed every week for 3 weeks. The fourth week
is patch-free, producing withdrawal bleeding. The effectiveness of Ortho Evra
is comparable to that of oral contraceptives. Its risks are similar to those of
oral contraceptives and include an increased risk of blood clots. The patch may
be applied to the torso, chest, arms, or thighs; it should not be applied to
the breasts.
NuvaRing
is a vaginal ring that is inserted in the vaginal for 3 weeks and then removed,
resulting in withdrawal bleeding. It is as effective as oral contraceptives and
has the same risks. It is flexible, does not require sizing or fitting, and is
effective when placed anywhere in the vagina.
Although
both of these contraceptive methods increase the options for women, neither
protects against STDs. Women using these methods should be instructed not to
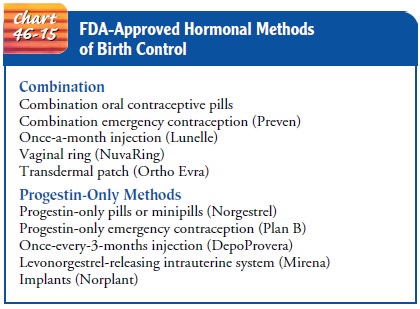
smoke. Chart 46-15 lists hormonal methods of birth control approved by the FDA.
Intrauterine Device
An IUD
is a small plastic device, usually T-shaped, that is inserted into the uterine
cavity to prevent pregnancy. A string attached to the IUD is visible and
palpable at the cervical os. An IUD pre-vents conception by causing a local
inflammatory reaction that is toxic to spermatozoa and blastocysts, thus
preventing fertiliza-tion. The IUD does not work by causing abortion.
Paraguard, a copper-bearing IUD, is effective for 10 years. Copper has an antispermatic effect. The Levonorgestrel Intra-uterine System (LNG-IUS; Mirena) is an IUD that releases levonorgestrel, a synthetic progestin used in oral contraceptives, and has been found to reduce heavy bleeding.
Limited studies show
that IUDs may prevent the need for hysterectomy in some women by reducing
bleeding, may be an adjunct in HRT, may protect women from endometrial cancer,
and may prevent cervi-cal cancer.
The
IUD method is effective over a long time, appears to have no systemic effects,
and reduces the possibility of patient error. This reversible method of birth
control is as effective as oral con-traceptives and more effective than barrier
methods.
Disadvantages
include possible excessive bleeding, cramps, and backaches and a slight risk of
tubal pregnancy, pelvic infec-tion, displacement of the device, and, rarely,
perforation of the cervix and uterus. If a pregnancy occurs with an IUD in
place, the device is removed immediately to avoid infection. Spontaneous
abortion (miscarriage) may occur on removal. An IUD is not usu-ally used in
women who have not had children because the nul-liparous uterus may be too
small to tolerate it. Women with multiple partners, women with heavy or crampy
periods, or those with a history of ectopic pregnancy or pelvic infection are
en-couraged to use other methods. Some clinicians test for chlamy-dia and
gonorrhea prior to insertion to prevent PID.
Mechanical Barriers
DIAPHRAGM
The
diaphragm is an effective contraceptive device that consists of a round,
flexible spring (50 to 90 mm wide) covered with a dome-like latex rubber cup. A
spermicidal (contraceptive) jelly or cream is used to coat the concave side of
the diaphragm before it is inserted deep into the vagina, covering the cervix.
The di-aphragm is a spermicide holder; the spermicide inhibits sperma-tozoa
from entering the cervical canal. The diaphragm is not felt by the user or her
partner when properly fitted and inserted. Be-cause women vary in size, the
diaphragm must be sized and fitted by an experienced clinician. The woman is
instructed in using and caring for the device. A return demonstration ensures
that the woman can insert the diaphragm correctly and that it covers the
cervix.
Each
time that the woman uses the diaphragm, she should ex-amine it carefully. By
holding it up to a bright light, she can en-sure that there are no pinpoint
holes, cracks, or tears in the diaphragm. Spermicidal jelly or cream is
applied, and the di-aphragm is then positioned to cover the cervix completely.
The diaphragm should remain in place at least 6 hours (but no more than 12
hours) after coitus. Additional spermicide is applied ifmore than 6 hours have
passed before intercourse occurs and before each act of intercourse. On
removal, the diaphragm is cleansed thoroughly with mild soap and water, rinsed,
and dried before it is stored in its original container.
Disadvantages
include allergic reactions in those who are sensi-tive to latex and an
increased incidence of urinary tract infections. Toxic shock syndrome has been
reported in some diaphragm users.
CERVICAL CAP
The
cervical cap is much smaller (22 to 35 mm) than the di-aphragm and covers only
the cervix; it is used with a spermicide. If a woman can feel her cervix, she
can usually learn to use a cer-vical cap. The chief advantage is that the cap
may be left in place for 2 days.
Although
convenient to use, the cervical cap may cause cervi-cal irritation; therefore,
before fitting a cap, most clinicians ob-tain a Pap smear and repeat the smear
after 3 months. The cap can stay in place for 48 hours and does not require
additional spermicide for repeated acts of intercourse.
FEMALE CONDOM
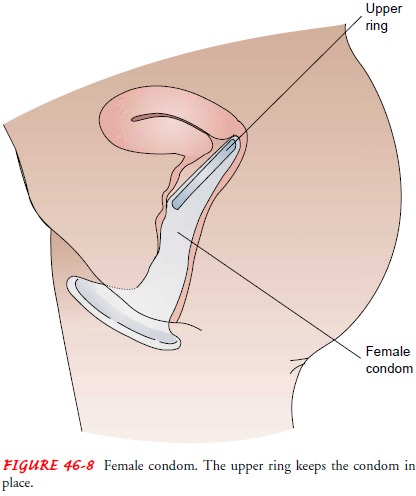
The female condom was developed to provide women with pro-tection from STDs and HIV as well as pregnancy. The female con-dom (Reality) consists of a cylinder of polyurethane enclosed at one end by a closed ring that covers the cervix and at the other end by an open ring that covers the perineum (Fig. 46-8). Advantages in-clude some degree of protection from STDs (HPV, herpes simplex virus, and HIV). Disadvantages include the inability to use the female condom with some coital positions (ie, standing).
SPERMICIDES
Spermicides
are available over the counter as foams, gels, and in-serts and on condoms.
Spermicides are effective, relatively inex-pensive chemical contraceptives when
used with condoms. When used alone, spermicide is better than no contraception
at all; it can be used without a partner’s cooperation and may provide
pro-tection from gonorrhea and chlamydia. Burning, a rash, or irri-tation can
develop in either partner and is usually temporary. Changing to another brand of
spermicide often alleviates the problem. Spermicides are made from nonoxynol-9
or octoxynol. Nonoxynol-9 has been found to be associated with minute tears in
vaginal tissue with frequent use, possibly increasing the possi-bility of
contracting HIV from an infected partner (Stephenson, 2000). It also may
increase the risk of latex allergy when used with a condom by leaching out a
natural rubber protein from the latex (Greydanus, Patel & Rimsza, 2001).
MALE CONDOM
The
male condom is an impermeable, snug-fitting cover applied to the erect penis
before it enters the vaginal canal. The tip of the condom is pinched while
being applied to leave space for ejacu-late. If no space is left, ejaculation
may cause a tear or hole in the condom and reduce its effectiveness. The penis,
with the condom held in place, is removed from the vagina while still erect to
pre-vent the ejaculate from leaking.
The
condom is an effective method when used with contra-ceptive foam. The latex
condom also creates a barrier against transmission of STDs, especially
gonorrhea, chlamydial infec-tion, and HIV. Natural condoms (those made from
animal tis-sue), however, do not protect against HIV infection. The nurse needs
to reassure women that they have a right to insist on their male partner using
a condom and a right to refuse sex without condoms, although women in abusive
relationships may increase their risk for abuse by doing so. Some women are
buying and car-rying condoms with them to be certain that one is available.
Nurses should be familiar and comfortable with instructions about using a
condom because many women need to know about this way of protecting themselves
from HIV and other STDs.
During
patient teaching about barrier methods of contracep-tion, nurses need to
consider the possibility of latex allergy for themselves and their patients.
Contact dermatitis is often the first symptom of latex allergy. Swelling and
itching can also occur. Pos-sible warning signs of latex allergy include oral
itching after blowing up a balloon or eating kiwis, bananas, pineapples,
passion fruits, avocados, or chestnuts. Because many contraceptives are made of
latex, patients who experience burning or itching while using a latex
contraceptive are instructed to see their primary health care provider.
Alternatives to latex condoms may include the female (Reality) and male
(Avanti) condoms made of polyurethane.
Condoms
do not provide complete protection from STDs, as the HPV virus may be
transmitted by skin-to-skin contact. Other STDs may be transmitted if any
abraded skin is exposed to body fluids. This information should be included in
patient teaching.
Coitus Interruptus
Coitus
interruptus (removing the penis from the vagina before ejaculation) requires
careful control by the male. Although it is a frequently used method of
preventing pregnancy, it is considered an unreliable method of contraception.
Rhythm and Natural Methods
Natural
family planning is any method of conception regulation that is based on
awareness of signs and symptoms of fertility dur-ing a menstrual cycle. The
advantages of natural contraceptive methods include the following: (1) they are
not hazardous to health, (2) they are inexpensive, and (3) they are approved by
some religions. The disadvantage is that they require discipline by the couple,
who must monitor the menstrual cycle and abstain from sex during the fertile
phase. In addition, the rhythm method of contraception can be difficult to use
because it relies on the woman determining her time of ovulation and on
avoiding in-tercourse during the fertile period. The fertile phase (which
re-quires sexual abstinence) is estimated to occur about 14 days before
menstruation, although it may occur between the 10th and 17th days. Spermatozoa
can fertilize an ovum up to 72 hours after intercourse, and the ovum can be
fertilized for 24 hours after leaving the ovary. The pregnancy rate with the
rhythm method is about 40% yearly.
Women
who carefully determine their “safe period,” based on a precise recording of
menstrual dates for at least 1 year, and who follow a carefully worked-out
formula may achieve very effective protection. A long abstinence period during
each cycle is required. These prerequisites require more time and control than
many cou-ples have. Changes in cervical mucus and basal body temperature due to
hormonal changes related to ovulation form the scientific basis for the
symptothermal method of ovulatory timing. Courses in natural family planning
are offered at many Catholic hospitals and some family planning clinics.
Ovulation
detection methods (eg, Ovulindex) are available in most pharmacies. The
presence of the enzyme guaiacol peroxi-dase in cervical mucus signals ovulation
6 days beforehand and also affects mucosal viscosity. Test kits are available
over the counter and are easy to use and reliable, but they can be expen-sive.
Ovulation prediction kits are more effective for planning conception than for
avoiding it.
Emergency Contraception
DOSE OF ESTROGEN/PROGESTIN
A
properly timed, adequate dose of estrogen or estrogen and a progestin after
intercourse without birth control, or when a method has failed, can prevent
pregnancy by inhibiting or delay-ing ovulation. This method does not interrupt
an established pregnancy. Nurses should be aware of this option and the indi-cations
for its use. This method obviously is not suitable for long-term contraception
because it is not as effective as daily oral contraceptives or other reliable
methods used regularly. However, it is valuable in emergency situations such as
rape, a defective or torn condom or diaphragm, or other situations that may
present the possibility of unwanted conception. It can be prescribed as Preven
(estrogen/progestin) or Plan B (progestin) packages of emergency contraception
with patient literature or it can be pre-scribed as a specific number of
contraceptive pills, depending on the medication and dose used.
Usually,
a small dose of oral contraceptives (ie, levonorgestrel and ethinyl estradiol)
is given and repeated in 12 hours (called the Yuzpe method after the
gynecologist who developed the method). This method must be used not more than
72 hours after inter-course. Nausea, a common side effect, can be minimized by
taking the medication with meals and with an antiemetic medication. Other side
effects, such as breast soreness and irregular bleeding, may occur but are
transient. Any patient using this method should
be
advised of the 1.6% failure rate and counseled about other con-traceptive
methods. Emergency contraception is related to luteal phase dysfunction,
producing an endometrium that is out of phase. There are no known
contraindications to the use of this method (Morris & Young, 2000).
The
nurse reviews with the patient instructions for taking the pills based on the
medication regimen prescribed. If the woman is breastfeeding, a progestin-only
formulation is prescribed. To avoid exposing the infant to synthetic hormones
through breast milk, she can manually express milk and bottle-feed for 24 hours
after treatment.
The
woman’s next menstrual period may begin a few days ear-lier or a few days later
than expected, and she needs to be in-formed of this. The patient must return
for a pregnancy test if she has not had a menstrual period in 3 weeks and
should be offered another visit to provide a regular method of contraception if
she does not have one currently. This medication may also be dis-pensed by
pharmacists without a prescription in some states. All women need to be aware
of this option and how to obtain it. Nurses can educate and inform women about
it to reduce un-wanted pregnancies and abortions.
POSTCOITAL IUD INSERTION
Postcoital
IUD insertion, another form of emergency contracep-tion, involves insertion of
a copper-bearing IUD within 5 days of exposure in women who want this method of
contraception; however, it may be inappropriate for some women or if other
contraindications exist. The mechanism of action is unknown, but it is thought
that the IUD interferes with fertilization (Mor-ris & Young, 2000). The
patient may experience discomfort on insertion and heavier menstrual periods
and increased cramping. Contraindications include a confirmed or suspected
pregnancy or any contraindication to regular copper IUD use. The patient must
be informed that there is a risk that insertion of an IUD may disrupt a
pregnancy that is already present.
NURSING MANAGEMENT
Patients
who use emergency contraception may be anxious, em-barrassed, and lacking
information about birth control. Nurses must be supportive and nonjudgmental
and provide facts and appropriate patient teaching. If a patient repeatedly
uses this method of birth control, she should be informed that the failure rate
with this method is higher than with a regularly used method. A toll-free
telephone information service (1-888-Not-2-Late) operates 24 hours a day in
English and Spanish and pro-vides information and referrals to health care
providers.
Related Topics