Chapter: Medical Physiology: Dominant Role of the Kidney in Long-Term Regulation of Arterial Pressure and in Hypertension: The Integrated System for Pressure Control
Components of the Renin-Angiotensin System
Components of the Renin-Angiotensin System
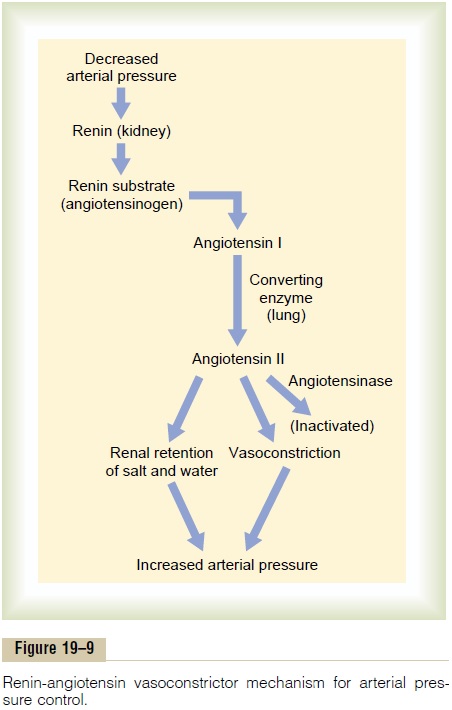
Figure 19–9 shows the functional steps by which the renin-angiotensin system helps to regulate arterial pressure.
Renin is synthesized and stored in an inactive form called prorenin in the juxtaglomerular cells (JG cells) of the kidneys. The JG cells are modified smooth muscle cells located in the walls of the afferent
arterioles immediately proximal to the glomeruli. Whenthe arterial pressure falls, intrinsic reactions in the kidneys themselves cause many of the prorenin mole-cules in the JG cells to split and release renin. Most of the renin enters the renal blood and then passes out of the kidneys to circulate throughout the entire body. However, small amounts of the renin do remain in the local fluids of the kidney and initiate several intrarenal functions.
Renin itself is an enzyme, not a vasoactive sub-stance. As shown in the schema of Figure 19–9, renin acts enzymatically on another plasma protein, a globulin called renin substrate (or angiotensinogen), to release a 10-amino acid peptide, angiotensin I. Angiotensin I has mild vasoconstrictor properties but not enough to cause significant changes in circulatory function. The renin persists in the blood for 30 minutes to 1 hour and continues to cause formation of still more angiotensin I during this entire time.
Within a few seconds to minutes after formation of angiotensin I, two additional amino acids are split from the angiotensin I to form the 8-amino acid peptide angiotensin II. This conversion occurs almost entirely in the lungs while the blood flows through the small vessels of the lungs, catalyzed by an enzyme called converting enzyme that is present in the endothelium of the lung vessels.
Angiotensin II is an extremely powerful vasocon-strictor, and it also affects circulatory function in other ways as well. However, it persists in the blood only for 1 or 2 minutes because it is rapidly inactivated by multiple blood and tissue enzymes collectively calledangiotensinases.
During its persistence in the blood, angiotensin II has two principal effects that can elevate arterial pressure. The first of these,vasoconstriction in manyareas of the body, occurs rapidly. Vasoconstrictionoccurs intensely in the arterioles and much less so in the veins. Constriction of the arterioles increases the total peripheral resistance, thereby raising the arterial pressure, as demonstrated at the bottom of the schema in Figure 19–9. Also, the mild constriction of the veins promotes increased venous return of blood to the heart, thereby helping the heart pump against the increasing pressure.
The second principal means by which angiotensin increases the arterial pressure is to decrease excretionof both salt and water by the kidneys. This slowlyincreases the extracellular fluid volume, which then increases the arterial pressure during subsequent hours and days. This long-term effect, acting through the extracellular fluid volume mechanism, is even more powerful than the acute vasoconstrictor mecha-nism in eventually raising the arterial pressure.
Rapidity and Intensity of the Vasoconstrictor Pressure Response to the Renin-Angiotensin System
Figure 19–10 shows a typical experiment demon-strating the effect of hemorrhage on the arterial pressure under two separate conditions: (1) with the renin-angiotensin system functioning and (2) without
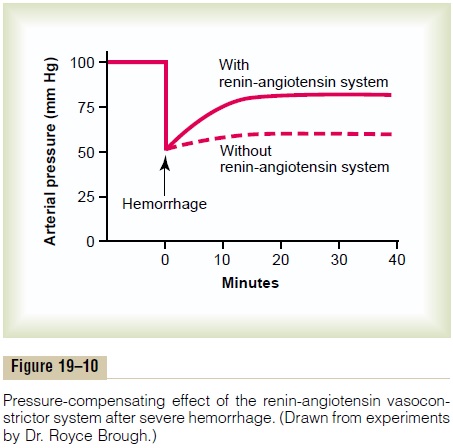
the system functioning (the system was interrupted by a renin-blocking antibody). Note that after hemor-rhage—enough to cause acute decrease of the arterial pressure to 50 mm Hg—the arterial pressure rose back to 83 mm Hg when the renin-angiotensin system was functional. Conversely, it rose to only 60 mm Hg when the renin-angiotensin system was blocked. This shows that the renin-angiotensin system is powerful enough to return the arterial pressure at least halfway back to normal within a few minutes after severe hemorrhage. Therefore, sometimes it can be of lifesaving service to the body, especially in circulatory shock.
Note also that the renin-angiotensin vasocon-strictor system requires about 20 minutes to become fully active. Therefore, it is somewhat slower to act for pressure control than are the nervous reflexes and the sympathetic norepinephrine-epinephrine system.
Effect of Angiotensin in the Kidneys to Cause Renal Retention of Salt and Water— An Especially Important Means for Long-Term Control of Arterial Pressure
Angiotensin causes the kidneys to retain both salt and water in two major ways:
1. Angiotensin acts directly on the kidneys to cause salt and water retention.
2.Angiotensin causes the adrenal glands to secrete aldosterone, and the aldosterone in turn increases salt and water reabsorption by the kidney tubules.
Thus, whenever excess amounts of angiotensin cir-culate in the blood, the entire long-term renal–body fluid mechanism for arterial pressure control auto-matically becomes set to a higher arterial pressure level than normal.
Mechanisms of the Direct Renal Effects of Angiotensin to Cause Renal Retention of Salt and Water. Angiotensin has severaldirect renal effects that make the kidneys retain salt and water. One major effect is to constrict the renal arterioles, thereby diminishing blood flow through the kidneys. As a result, less fluid filters through the glomeruli into the tubules. Also, the slow flow of blood reduces the pressure in the peritubular capillaries, which causes rapid reabsorption of fluid from the tubules. And still a third effect is that angiotensin has important direct actions on the tubular cells them-selves to increase tubular reabsorption of sodium and water. The total result of all these effects is significant, sometimes decreasing urine output less than one fifth of normal.
Stimulation of Aldosterone Secretion by Angiotensin, and the Effect of Aldosterone in Increasing Salt and Water Retention by the Kidneys. Angiotensin is also one of the mostpowerful stimulators of aldosterone secretion by the adrenal glands, as we shall discuss in relation to body fluid regulation and in relation to adrenal gland function. Therefore, when the renin-angiotensin system becomes activated, the rate of aldosterone secretion usually also increases; and an important subsequent function of aldosterone is to cause marked increase in sodium reabsorption by the kidney tubules, thus increasing the total body extracellular fluid sodium. This increased sodium then causes water retention, as already explained, increas-ing the extracellular fluid volume and leading second-arily to still more long-term elevation of the arterial pressure.
Thus both the direct effect of angiotensin on the kidney and its effect acting through aldosterone are important in long-term arterial pressure control. However, research in our own laboratory has sug-gested that the direct effect of angiotensin on the kidneys is perhaps three or more times as potent as the indirect effect acting through aldosterone—even though the indirect effect is the one most widely known.
Quantitative Analysis of Arterial Pressure Changes Caused by Angiotensin. Figure 19–11 shows a quantitative analysisof the effect of angiotensin in arterial pressure control. This figure shows two renal output curves as well as a line depicting normal level of sodium intake. The left-hand renal output curve is that measured in dogs whose renin-angiotensin system had been blocked by the drugcaptopril (which blocks the conversion of angiotensin Ito angiotensin II, the active form of angiotensin). The right-hand curve was measured in dogs infused contin-uously with angiotensin II at a level about 2.5 times the normal rate of angiotensin formation in the blood. Note the shift of the renal output curve toward higher pres-sure levels under the influence of angiotensin II. This shift is caused by both the direct effects of angiotensin on the kidney and the indirect effect acting through aldosterone secretion, as explained above.
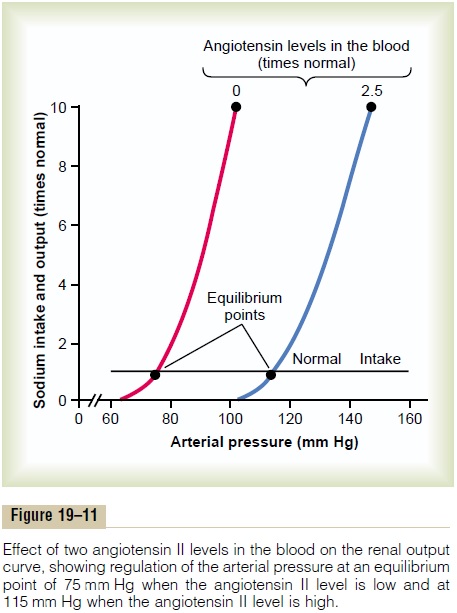
Finally, note the two equilibrium points, one for zero angiotensin showing an arterial pressure level of 75 mm Hg, and one for elevated angiotensin showing a pressure level of 115 mm Hg. Therefore, the effect of angiotensin to cause renal retention of salt and water can have a powerful effect in promoting chronic eleva-tion of the arterial pressure.
Role of the Renin-Angiotensin System in Maintaining a Normal Arterial Pressure Despite Wide Variations in Salt Intake
One of the most important functions of the renin-angiotensin system is to allow a person to eat either very small or very large amounts of salt without causing great changes in either extracellular fluid volume or arterial pressure. This function is explained by the schema in Figure 19–12, which shows that the initial effect of increased salt intake is to elevate the extracellular fluid volume and this in turn to elevate the arterial pressure. Then, the increased arterial pres-sure causes increased blood flow through the kidneys, which reduces the rate of secretion of renin to a much lower level and leads sequentially to decreased renal retention of salt and water, return of the extracellular fluid volume almost to normal, and, finally, return of the arterial pressure also almost to normal. Thus, the renin-angiotensin system is an automatic feedback mechanism that helps maintain the arterial pressure at or near the normal level even when salt intake is increased. Or, when salt intake is decreased below normal, exactly opposite effects take place.
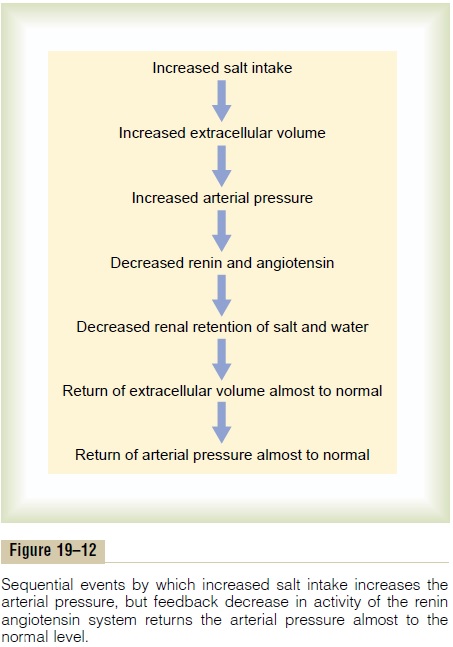
To emphasize the efficacy of the renin-angiotensin system in controlling arterial pressure, when the system functions normally, the pressure rises no more increase in salt intake. Conversely, when the renin- angiotensin system is blocked, the same increase in salt intake sometimes causes the pressure to rise 10 times the normal increase, often as much as 50 to 60 mm Hg.
Related Topics