Chapter: Basic & Clinical Pharmacology : Antipsychotic Agents & Lithium
Clinical Pharmacology of Antipsychotic Agents
CLINICAL PHARMACOLOGY OF ANTIPSYCHOTIC AGENTS
Indications
A. Psychiatric Indications
Schizophrenia is the primary indication for antipsychotic agents.Antipsychotic drugs are also used very extensively in patients with psychotic bipolar disorder (BP1), psychotic depression, and treatment-resistant depression.
Catatonic forms of schizophrenia are best managed by intrave-nous benzodiazepines. Antipsychotic drugs may be needed to treat psychotic components of that form of the illness after catatonia has ended, and they remain the mainstay of treatment for this condition. Unfortunately, many patients show little response, and virtually none show a complete response.
Antipsychotic drugs are also indicated for schizoaffectivedisorders, which share characteristics of both schizophrenia andaffective disorders. No fundamental difference between these two diagnoses has been reliably demonstrated. It is most likely that they are part of a continuum with bipolar psychotic disor-der. The psychotic aspects of the illness require treatment with antipsychotic drugs, which may be used with other drugs such as antidepressants, lithium, or valproic acid. The manic phase in bipolar affective disorder often requires treatment with anti-psychotic agents, although lithium or valproic acid supple-mented with high-potency benzodiazepines (eg, lorazepam or clonazepam) may suffice in milder cases. Recent controlled trials support the efficacy of monotherapy with atypical antipsychotics in the acute phase (up to 4 weeks) of mania. Aripiprazole, olanzapine, quetiapine, risperidone and ziprasidone have been approved for treatment of various phases of bipolar disorder. They are most effective for the manic phase and for maintenance treatment.
As mania subsides, the antipsychotic drug may be withdrawn, although maintenance treatment with atypical antipsychotic agents has become more common. Nonmanic excited states may also be managed by antipsychotics, often in combination with benzodiazepines.
Other indications for the use of antipsychotics include Tourette’ssyndrome, disturbed behavior in patients withAlzheimer’s disease, and, with antidepressants, psychotic depression. Antipsychotics are not indicated for the treatment of various withdrawal syndromes, eg, opioid withdrawal. In small doses, antipsychotic drugs have been promoted (wrongly) for the relief of anxiety associated with minor emotional disorders. The antianxiety sedatives are preferred in terms of both safety and acceptability to patients.
B. Nonpsychiatric Indications
Most older typical antipsychotic drugs, with the exception of thi-oridazine, have a strong antiemetic effect. This action is due to dopamine-receptor blockade, both centrally (in the chemorecep-tor trigger zone of the medulla) and peripherally (on receptors in the stomach). Some drugs, such as prochlorperazine and benz-quinamide, are promoted solely as antiemetics.
Phenothiazines with shorter side chains have considerable H1-receptor-blocking action and have been used for relief of pruritusor, in the case of promethazine, as preoperative sedatives. The butyrophenone droperidol is used in combination with an opioid, fentanyl, in neuroleptanesthesia.
Drug Choice
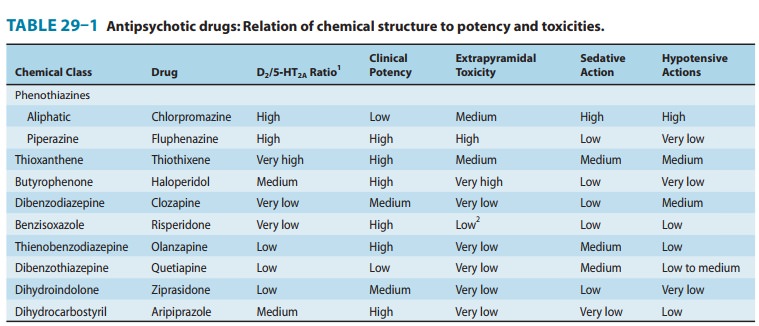
Choice among antipsychotic drugs is based mainly on differences in adverse effects and possible differences in efficacy. Since use of the older drugs is still widespread, especially for patients treated in the public sector, knowledge of such agents as chlorpromazine and haloperidol remains relevant. Thus, one should be familiar with one member of each of the three subfamilies of phenothiazines, a member of the thioxanthene and butyrophenone group, and all of the newer compounds—clozapine, risperidone, olanzapine, que-tiapine, ziprasidone, and aripiprazole. Each may have special benefits for selected patients. A representative group of antipsy-chotic drugs is presented in Table 29–3.
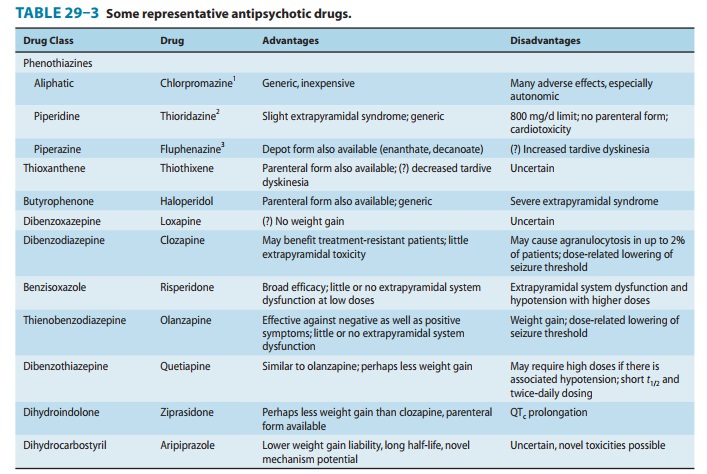
For approximately 70% of patients with schizophrenia, and probably for a similar proportion of patients with bipolar disorder with psychotic features, typical and atypical antipsychotic drugs are of equal efficacy for treating positive symptoms. However, the evidence favors atypical drugs for benefit for negative symptoms and cognition, for diminished risk of tardive dyskinesia and other forms of EPS, and for lesser increases in prolactin levels.
Some of the atypical antipsychotic drugs produce more weight gain and increases in lipids than some typical antipsychotic drugs. A small percentage of patients develop diabetes mellitus, most often seen with clozapine and olanzapine. Ziprasidone is the atypical drug causing the least weight gain. Risperidone, paliperidone, and aripip-razole usually produce small increases in weight and lipids. Asenapine and quetiapine have an intermediate effect. Clozapine and olanzapine frequently result in large increases in weight and lipids. Thus, these drugs should be considered as second-line drugs unless there is a specific indication. That is the case with clozapine, which at high doses (300–900 mg/d) is effective in the majority of patients with schizophrenia refractory to other drugs, provided that treatment is continued for up to 6 months. Case reports and several clinical trials suggest that high-dose olanzapine, ie, doses of 30–45 mg/d, may also be efficacious in refractory schizophrenia when given over a 6-month period. Clozapine is the only atypical anti-psychotic drug indicated to reduce the risk of suicide. All patients with schizophrenia who have made life-threatening suicide attempts should be seriously evaluated for switching to clozapine.
New antipsychotic drugs have been shown in some trials to be more effective than older ones for treating negative symptoms. The floridly psychotic form of the illness accompanied by uncon-trollable behavior probably responds equally well to all potent antipsychotics but is still frequently treated with older drugs that offer intramuscular formulations for acute and chronic treat-ment. Moreover, the low cost of the older drugs contributes to their widespread use despite their risk of adverse EPS effects. Several of the newer antipsychotics, including clozapine, risperi-done, and olanzapine, show superiority over haloperidol in terms of overall response in some controlled trials. More comparative studies with aripiprazole are needed to evaluate its relative effi-cacy. Moreover, the superior adverse-effect profile of the newer agents and low to absent risk of tardive dyskinesia suggest that these should provide the first line of treatment.
The best guide for selecting a drug for an individual patient is the patient’s past responses to drugs. At present, clozapine is limited to those patients who have failed to respond to substan-tial doses of conventional antipsychotic drugs. The agranulocy-tosis and seizures associated with this drug prevent more widespread use. Risperidone’s superior side-effect profile (com-pared with that of haloperidol) at dosages of 6 mg/d or less and the lower risk of tardive dyskinesia have contributed to its wide-spread use. Olanzapine and quetiapine may have even lower risk and have also achieved widespread use.
Dosage
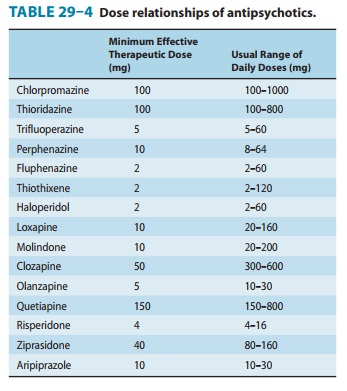
The range of effective dosages among various antipsychotic agents is broad. Therapeutic margins are substantial. At appropriate dosages, antipsychotics—with the exception of clozapine and per-haps olanzapine—are of equal efficacy in broadly selected groups of patients. However, some patients who fail to respond to one drug may respond to another; for this reason, several drugs may have to be tried to find the one most effective for an individual patient. Patients who have become refractory to two or three antipsychotic agents given in substantial doses become candidates for treatment with clozapine or high-dose olanzapine. Thirty to fifty percent of patients previously refractory to standard doses of other antipsychotic drugs respond to these drugs. In such cases, the increased risk of clozapine can well be justified.Some dosage relationships between various antipsychotic drugs, as well as possible therapeutic ranges, are shown in Table 29–4.
Parenteral Preparations
Well-tolerated parenteral forms of the high-potency older drugs haloperidol and fluphenazine are available for rapid initiation of treatment as well as for maintenance treatment in noncompliant patients. Since the parenterally administered drugs may have much greater bioavailability than the oral forms, doses should be only a fraction of what might be given orally, and the manufacturer’s lit-erature should be consulted. Fluphenazine decanoate and haloperi-dol decanoate are suitable for long-term parenteral maintenance therapy in patients who cannot or will not take oral medication.
Dosage Schedules
Antipsychotic drugs are often given in divided daily doses, titrat-ing to an effective dosage. The low end of the dosage range in Table 29–4 should be tried for at least several weeks. After an effective daily dosage has been defined for an individual patient, doses can be given less frequently. Once-daily doses, usually given at night, are feasible for many patients during chronic mainte-nance treatment. Simplification of dosage schedules leads to better compliance.
Maintenance Treatment
A very small minority of schizophrenic patients may recover from an acute episode and require no further drug therapy for pro-longed periods. In most cases, the choice is between “as needed” increased doses or the addition of other drugs for exacerbations versus continual maintenance treatment with full therapeutic dos-age. The choice depends on social factors such as the availability of family or friends familiar with the symptoms of early relapse and ready access to care.
Drug Combinations
Combining antipsychotic drugs confounds evaluation of the efficacy of the drugs being used. Use of combinations, how-ever, is widespread, with more emerging experimental data supporting such practices. Tricyclic antidepressants or, more often, selective serotonin reuptake inhibitors (SSRIs) are often used with antipsychotic agents for symptoms of depression complicating schizophrenia. The evidence for the usefulness of this polypharmacy is minimal. Electroconvulsive therapy (ECT) is a useful adjunct for antipsychotic drugs, not only for treating mood symptoms, but for positive symptom control as well. Electroconvulsive therapy can augment clozapine when maximum doses of clozapine are ineffective. In contrast, add-ing risperidone to clozapine is not beneficial. Lithium or valp-roic acid is sometimes added to antipsychotic agents with benefit to patients who do not respond to the latter drugs alone. There is some evidence that lamotrigine is more effective than any of the other mood stabilizers for this indication . It is uncertain whether instances of successful combi-nation therapy represent misdiagnosed cases of mania or schizoaffective disorder. Benzodiazepines may be useful for patients with anxiety symptoms or insomnia not controlled by antipsychotics.
Adverse Reactions
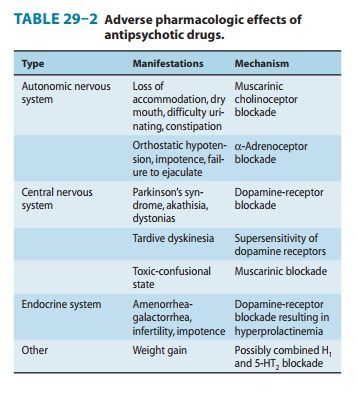
Most of the unwanted effects of antipsychotic drugs are extensions of their known pharmacologic actions (Tables 29–1 and 29–2), but a few effects are allergic in nature and some are idiosyncratic.
A. Behavioral Effects
The older typical antipsychotic drugs are unpleasant to take. Many patients stop taking these drugs because of the adverse effects, which may be mitigated by giving small doses during the day and the major portion at bedtime. A “pseudodepression” that may be due to drug-induced akinesia usually responds to treat-ment with antiparkinsonism drugs. Other pseudodepressions may be due to higher doses than needed in a partially remitted patient,in which case decreasing the dose may relieve the symptoms. Toxic-confusional states may occur with very high doses of drugs that have prominent antimuscarinic actions.
B. Neurologic Effects
Extrapyramidal reactions occurring early during treatment with older agents include typical Parkinson’s syndrome, akathisia (uncontrollable restlessness), and acute dystonic reactions (spastic retrocollis or torticollis). Parkinsonism can be treated, when neces-sary, with conventional antiparkinsonism drugs of the antimuscar-inic type or, in rare cases, with amantadine. (Levodopa should never be used in these patients.) Parkinsonism may be self-limiting, so that an attempt to withdraw antiparkinsonism drugs should be made every 3–4 months. Akathisia and dystonic reactions also respond to such treatment, but many clinicians prefer to use a seda-tive antihistamine with anticholinergic properties, eg, diphenhy-dramine, which can be given either parenterally or orally.
Tardive dyskinesia, as the name implies, is a late-occurringsyndrome of abnormal choreoathetoid movements. It is the most important unwanted effect of antipsychotic drugs. It has been proposed that it is caused by a relative cholinergic defi-ciency secondary to supersensitivity of dopamine receptors in the caudate-putamen. The prevalence varies enormously, but tardive dyskinesia is estimated to have occurred in 20–40% of chronically treated patients before the introduction of the newer atypical antipsychotics. Early recognition is important, since advanced cases may be difficult to reverse. Any patient with tardive dyskinesia treated with a typical antipsychotic drug or possibly risperidone or paliperidone should be switched to quetiapine or clozapine, the atypical agents with the least likelihood of causing tardive dyskinesia. Many treatments have been proposed, but their evaluation is confounded by the fact that the course of the disorder is variable and sometimes self-limited. Reduction in dosage may also be considered. Most authorities agree that the first step should be to discontinue or reduce the dose of the current antipsychotic agent or switch to one of the newer atypical agents. A logical second step would be to eliminate all drugs with central anticholinergic action, particularly antiparkinsonism drugs and tricyclic antidepres-sants. These two steps are often enough to bring about improvement. If they fail, the addition of diazepam in doses as high as 30–40 mg/d may add to the improvement by enhanc-ing GABAergic activity.
Seizures, though recognized as a complication of chlorprom-azine treatment, were so rare with the high-potency older drugs as to merit little consideration. However, de novo seizures may occur in 2–5% of patients treated with clozapine. Use of an anticonvul-sant is able to control seizures in most cases.
C. Autonomic Nervous System Effects
Most patients are able to tolerate the antimuscarinic adverse effects of antipsychotic drugs. Those who are made too uncom-fortable or who develop urinary retention or other severe symp-toms can be switched to an agent without significant antimuscarinic action. Orthostatic hypotension or impaired ejaculation—common complications of therapy with chlorprom-azine or mesoridazine—should be managed by switching to drugs with less marked adrenoceptor-blocking actions.
D. Metabolic and Endocrine Effects
Weight gain is very common, especially with clozapine and olan-zapine, and requires monitoring of food intake, especially carbohy-drates. Hyperglycemia may develop, but whether secondary to weight gain-associated insulin resistance or to other potential mechanisms remains to be clarified. Hyperlipidemia may occur. The management of weight gain, insulin resistance, and increased lipids should include monitoring of weight at each visit and mea-surement of fasting blood sugar and lipids at 3–6 month intervals. Measurement of hemoglobin A1C may be useful when it is impos-sible to be sure of obtaining a fasting blood sugar. Diabetic ketoac-idosis has been reported in a few cases. The triglyceride:HDL ratio should be less than 3.5 in fasting samples. Levels higher than that indicate increased risk of atherosclerotic cardiovascular disease.
Hyperprolactinemia in women results in the amenorrhea-galactorrhea syndrome and infertility; in men, loss of libido, impo-tence, and infertility may result. Hyperprolactinemia may cause osteoporosis, particularly in women. If dose reduction is not indi-cated, or ineffective in controlling this pattern, switching to one of the atypical agents that do not raise prolactin levels, eg, aripiprazole, may be indicated.
E. Toxic or Allergic Reactions
Agranulocytosis, cholestatic jaundice, and skin eruptions occur rarely with the high-potency antipsychotic drugs currently used.In contrast to other antipsychotic agents, clozapine causes agranulocytosis in a small but significant number of patients— approximately 1–2% of those treated. This serious, potentially fatal effect can develop rapidly, usually between the 6th and 18th weeks of therapy. It is not known whether it represents an immune reaction, but it appears to be reversible upon discontinuance of the drug. Because of the risk of agranulocytosis, patients receivingclozapine must have weekly blood counts for the first 6 months of treatment and every 3 weeks thereafter.
F. Ocular Complications
Deposits in the anterior portions of the eye (cornea and lens) are a common complication of chlorpromazine therapy. They may accentuate the normal processes of aging of the lens. Thioridazine is the only antipsychotic drug that causes retinal deposits, which in advanced cases may resemble retinitis pigmentosa. The deposits are usually associated with “browning” of vision. The maximum daily dose of thioridazine has been limited to 800 mg/d to reduce the possibility of this complication.
G. Cardiac Toxicity
Thioridazine in doses exceeding 300 mg daily is almost always associated with minor abnormalities of T waves that are easily reversible. Overdoses of thioridazine are associated with major ventricular arrhythmias, eg, torsades de pointes, cardiac conduc-tion block, and sudden death; it is not certain whether thioridazine can cause these same disorders when used in therapeutic doses. In view of possible additive antimuscarinic and quinidine-like actions with various tricyclic antidepressants, thioridazine should be com-bined with the latter drugs only with great care. Among the atypical agents, ziprasidone carries the greatest risk of QT prolon-gation and therefore should not be combined with other drugs that prolong the QT interval, including thioridazine, pimozide, and group 1A or 3 antiarrhythmic drugs. Clozapine is sometimes associated with myocarditis and must be discontinued if myo-carditis manifests. Sudden death due to arrhythmias is common in schizophrenia. It is not always drug-related, and there are no stud-ies that definitively show increased risk with particular drugs. Monitoring of QTc prolongation has proved to be of little use unless the values increase to more than 500 ms and this is mani-fested in multiple rhythm strips or a Holter monitor study. A 20,000 patient study of ziprasidone versus olanzapine showed minimal or no increased risk of torsades de pointes or sudden death in patients who were randomized to ziprasidone.
H. Use in Pregnancy; Dysmorphogenesis
Although antipsychotic drugs appear to be relatively safe in preg-nancy, a small increase in teratogenic risk could be missed. Questions about whether to use these drugs during pregnancy and whether to abort a pregnancy in which the fetus has already been exposed must be decided individually. If a pregnant woman could manage to be free of antipsychotic drugs during pregnancy, this would be desirable because of their effects on the neurotransmit-ters involved in neurodevelopment.
I. Neuroleptic Malignant Syndrome
This life-threatening disorder occurs in patients who are extremely sensitive to the extrapyramidal effects of antipsychotic agents. The initial symptom is marked muscle rigidity. If sweating is impaired, as it often is during treatment with anti-cholinergic drugs, fever may ensue, often reaching dangerous lev-els. The stress leukocytosis and high fever associated with this syndrome may erroneously suggest an infectious process. Autonomic instability, with altered blood pressure and pulse rate, is often present.
Muscle-type creatine kinase levels are usually elevated, reflect-ing muscle damage. This syndrome is believed to result from an excessively rapid blockade of postsynaptic dopamine receptors. A severe form of extrapyramidal syndrome follows. Early in the course, vigorous treatment of the extrapyramidal syndrome with antiparkinsonism drugs is worthwhile. Muscle relaxants, particu-larly diazepam, are often useful. Other muscle relaxants, such as dantrolene, or dopamine agonists, such as bromocriptine, have been reported to be helpful. If fever is present, cooling by physical measures should be tried. Various minor forms of this syndrome are now recognized. Switching to an atypical drug after recovery is indicated.
Drug Interactions
Antipsychotics produce more important pharmacodynamic than pharmacokinetic interactions because of their multiple effects Additive effects may occur when these drugs are combined with others that have sedative effects, α-adrenoceptor–blocking action, anticholinergic effects, and—for thioridazine and ziprasidone— quinidine-like action.
A variety of pharmacokinetic interactions have been reported, but none are of major clinical significance.
Overdoses
Poisonings with antipsychotic agents (unlike tricyclic antidepres-sants) are rarely fatal, with the exception of those due to mesoridazine and thioridazine. In general, drowsiness proceeds to coma, with an intervening period of agitation. Neuromuscular excitability may be increased and proceed to convulsions. Pupils are miotic, and deep tendon reflexes are decreased. Hypotension and hypothermia are the rule, although fever may be present later in the course. The lethal effects of mesoridazine and thioridazine are related to induction of ventricular tachyarrhythmias. Patients should be given the usual “ABCD” treatment for poisonings and treated supportively. Management of overdoses of thioridazine and mesoridazine, which are complicated by car-diac arrhythmias, is similar to that for tricyclic antidepressants .
Psychosocial Treatment & Cognitive Remediation
Patients with schizophrenia need psychosocial support based around activities of daily living, including housing, social activities, returning to school, obtaining the optimal level of work they may be capable of, and restoring social interactions. Unfortunately, funding for this crucial component of treat-ment has been minimized in recent years. Case management and therapy services are a vital part of the treatment program that should be provided to patients with schizophrenia. First-episode patients are particularly needful of this support because they often deny their illness and are noncompliant with medication.
Benefits & Limitations of Drug Treatment
As noted at the beginningr, antipsychotic drugs have had a major impact on psychiatric treatment. First, they have shifted the vast majority of patients from long-term hospi-talization to the community. For many patients, this shift has provided a better life under more humane circumstances and in many cases has made possible life without frequent use of physi-cal restraints. For others, the tragedy of an aimless existence is now being played out in the streets of our communities rather than in mental institutions.
Second, these antipsychotic drugs have markedly shifted psy-chiatric thinking to a more biologic orientation. Partly because of research stimulated by the effects of these drugs on schizophrenia, we now know much more about central nervous system physiol-ogy and pharmacology than was known before the introduction of these agents. However, despite much research, schizophreniaremains a scientific mystery and a personal disaster for the patient. Although most schizophrenic patients obtain some degree of ben-efit from these drugs—in some cases substantial benefit—none are made well by them.
Related Topics