Chapter: Modern Pharmacology with Clinical Applications: Pharmacological Management of Chronic Heart Failure
Classification of Antiarrhythmic Drugs
CLASSIFICATION
OF ANTIARRHYTHMIC DRUGS
Antiarrhythmic drugs have
historically been segre-gated by the Vaughn Williams classification system into
four main groups, based on their predominant mecha-nism of action. This is a
good starting point for organ-izing one’s thinking about the various antiarrhythmic
drugs, but it is a great oversimplification and does not address several drugs
that have electrophysiological effects characteristic of more than one group.
Thus, although the grouping of antiarrhythmic agents into four classes is
convenient, such a classification falls short of explaining the underlying
mechanisms by which many drugs ultimately exert their therapeutic
antiarrhythmic effect. Also, certain agents do not fall neatly into the four
classes;.
Class I Drugs
Class I antiarrhythmic drugs
are characterized by their ability to block the voltage-gated sodium channel.
The class I agents may block the channel when it is in either the open or the
inactivated state. Inhibition of the sodium channel results in a decrease in
the rate of rise of phase 0 of the cardiac membrane action potential and a
slowing of the conduction velocity. Additionally, class I drugs, through
inhibition of the sodium channel, require that a more hyperpolarized membrane
poten-tial (more negative) be achieved before the membrane becomes excitable
and can propagate an excitatory stimulus. As a result, the ERP of fast-response
fibers is prolonged. Although many class I antiarrhythmic drugs possess local
anesthetic actions and can depress myo-cardial contractile force, these effects
are usually ob-served only at higher plasma concentrations.
The antiarrhythmic drugs in class I suppress both normal Purkinje
fiber and His bundle automaticity in addition to abnormal automaticity
resulting from myo-cardial damage. Suppression of abnormal automaticity permits the sinoatrial node again to
assume the role of the dominant pacemaker.
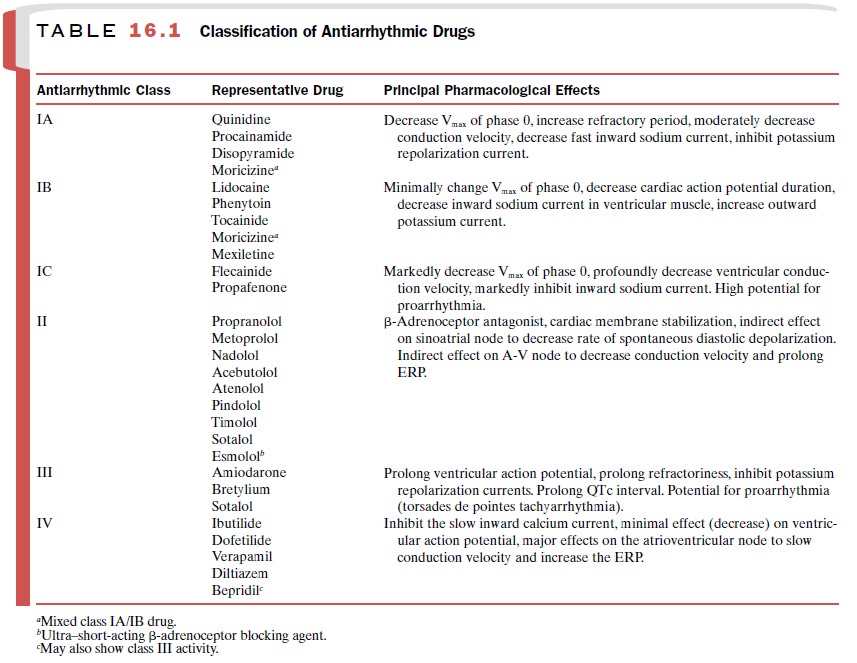
The antiarrhythmic agents
that belong to class I are divided into three subgroups (Table 16.1) with
slightly different properties. Class IA drugs slow the rate of rise of phase 0
(Vmax>) of the action potential and prolong the ventricular ERP.
Members of this class impair the function of the membrane sodium channel,
thereby de-creasing the number of channels available for mem-brane
depolarization. Class IA drugs do not alter the resting membrane potential.
Because they decrease Vmax>, class IA drugs slow conduction
velocity. Members of this class directly decrease the slope of phase 4
depo-larization in pacemaker cells, especially those that arise outside of the
sinoatrial node.
Members of class IB have a
minimal effect on the rate of depolarization and are characterized by their
ability to decrease the duration of action potential and ERP of Purkinje
fibers. Members of this class have a minimal effect on conduction velocity in
ventricular myocardium and are without apparent effect on refrac-toriness.
The drugs in class IC produce
a marked depression in the rate of rise of the membrane action potential and
have minimal effects on the duration of membrane ac-tion potential and ERP of
ventricular myocardial cells.
Class II Drugs
Class II antiarrhythmic drugs competitively inhibit β- adrenoceptors and inhibit
catecholamine-induced stimu-lation of cardiac β-receptors. In addition, some members of the group (e.g., propranolol and
acebutolol) cause electrophysiological alterations in Purkinje fibers that
resemble those produced by class I antiarrhythmic drugs. The latter actions
have been called membrane-stabilizing effects.
Class III Drugs
Class III antiarrhythmic drugs prolong the membrane action potential by delaying repolarization without alter-ing phase 0 of depolarization or the resting membrane potential. Class III drugs have a significant risk of proar-rhythmia because of the prolongation of action poten-tial and the induction of torsades de pointes.
Class IV Drugs
Class IV drugs block the slow inward Ca++ current (L-type calcium channel) in
cardiac tissue. The most pro-nounced electrophysiological effects are
exerted on car-diac cells that depend on the Ca++ channel for
initiating the action potential, such as those found in the sinoatrial and A-V
nodes. The administration of class IV drugs slows conduction velocity and
increases refractoriness in the A-V node, thereby reducing the ability of the
A-V node to conduct rapid impulses to the ventricle. This ac-tion may terminate
supraventricular tachycardias and can slow conduction during atrial flutter or
fibrillation.
Related Topics