Chapter: Medical Physiology: Dominant Role of the Kidney in Long-Term Regulation of Arterial Pressure and in Hypertension: The Integrated System for Pressure Control
Chronic Hypertension (High Blood Pressure) Is Caused by Impaired Renal Fluid Excretion
Chronic Hypertension (High Blood Pressure) Is Caused by Impaired Renal Fluid Excretion
When a person is said to have chronic hypertension (or “high blood pressure”), it is meant that his or her meanarterial pressure is greater than the upper range of theaccepted normal measure. A mean arterial pressure greater than 110 mm Hg (normal is about 90 mm Hg) is considered to be hypertensive. (This level of mean pressure occurs when the diastolic blood pressure is greater than about 90 mm Hg and the systolic pressure is greater than about 135 mm Hg.) In severe hyper-tension, the mean arterial pressure can rise to 150 to 170 mm Hg, with diastolic pressure as high as 130 mm Hg and systolic pressure occasionally as high as 250 mm Hg.
Even moderate elevation of arterial pressure leads to shortened life expectancy. At severely high pres-sures—mean arterial pressures 50 per cent or more above normal—a person can expect to live no more than a few more years unless appropriately treated.
The lethal effects of hypertension are caused mainly in three ways:
1. Excess workload on the heart leads to early heart failure and coronary heart disease, often causing death as a result of a heart attack.
2. The high pressure frequently damages a major blood vessel in the brain, followed by death of
Clinically it is called a “stroke.” Dependingon which part of the brain is involved, a stroke can cause paralysis, dementia, blindness, or multiple other serious brain disorders.
3. High pressure almost always causes injury in the kidneys, producing many areas of renal destruction and, eventually, kidney failure, uremia, and death.
Lessons learned from the type of hypertension called “volume-loading hypertension” have been crucial in understanding the role of the renal–body fluid volume mechanism for arterial pressure regula-tion. Volume-loading hypertension means hyperten-sion caused by excess accumulation of extracellular fluid in the body, some examples of which follow.
Experimental Volume-Loading Hypertension Caused by Reduced Renal Mass Along with Simultaneous Increase in Salt Intake.
Figure 19–7 shows a typical experiment demonstrating volume-loading hypertension in a group of dogs with 70 per cent of their kidney mass removed. At the first circled point on the curve, the two poles of one of the kidneys were removed, and at the second circled point, the entire opposite kidney was removed, leaving the animals with only 30 per cent of normal renal mass. Note that removal of this amount of kidney mass increased the arterial pressure an average of only 6 mm Hg. Then, the dogs were given salt solution to drink instead of water. Because salt solution fails to quench the thirst, the dogs drank two to four times the normal amounts of volume, and within a few days, their average arterial pressure rose to about 40 mm Hg above normal. After 2 weeks, the dogs were given tap water again instead of salt solution; the pressure returned to normal within 2 days. Finally, at the end of the experiment, the dogs were given salt solution again, and this time the pressure rose much more rapidly to an even higher level because the dogs had already learned to tolerate the salt solution and there-fore drank much more. Thus, this experiment demon-strates volume-loading hypertension.
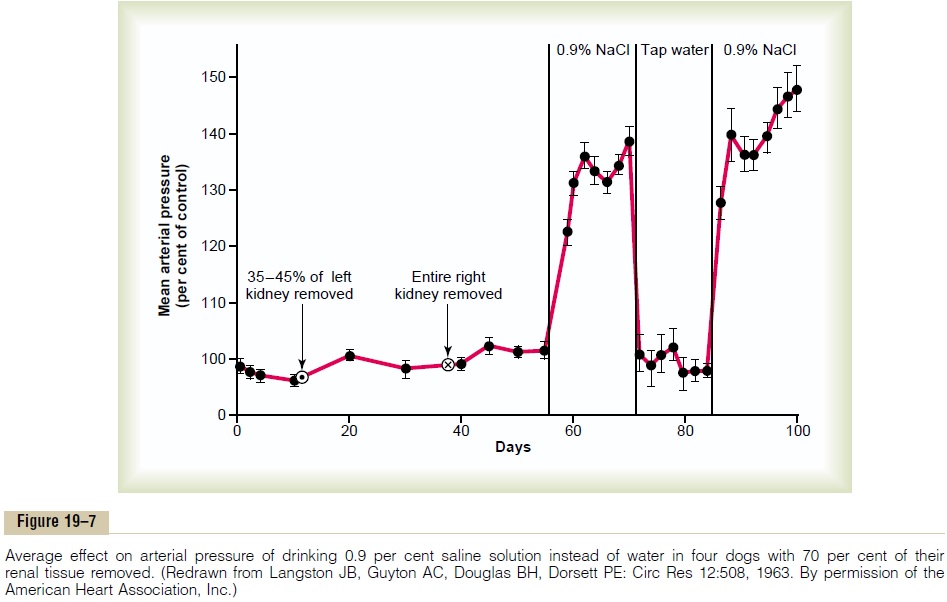
If the reader considers again the basic determinants of long-term arterial pressure regulation, he or she can immediately understand why hypertension occurred in the volume-loading experiment of Figure 19–7. First, reduction of the kidney mass to 30 per cent of normal greatly reduced the ability of the kidneys to excrete salt and water. Therefore, salt and water accumulated in the body and in a few days raised the arterial pres-sure high enough to excrete the excess salt and water intake.
Sequential Changes in Circulatory Function During the Devel-opment of Volume-Loading Hypertension. It is especiallyinstructive to study the sequential changes in circula-tory function during progressive development of volume-loading hypertension. Figure 19–8 shows these sequential changes. A week or so before the point labeled “0” days, the kidney mass had already been decreased to only 30 per cent of normal. Then, at this
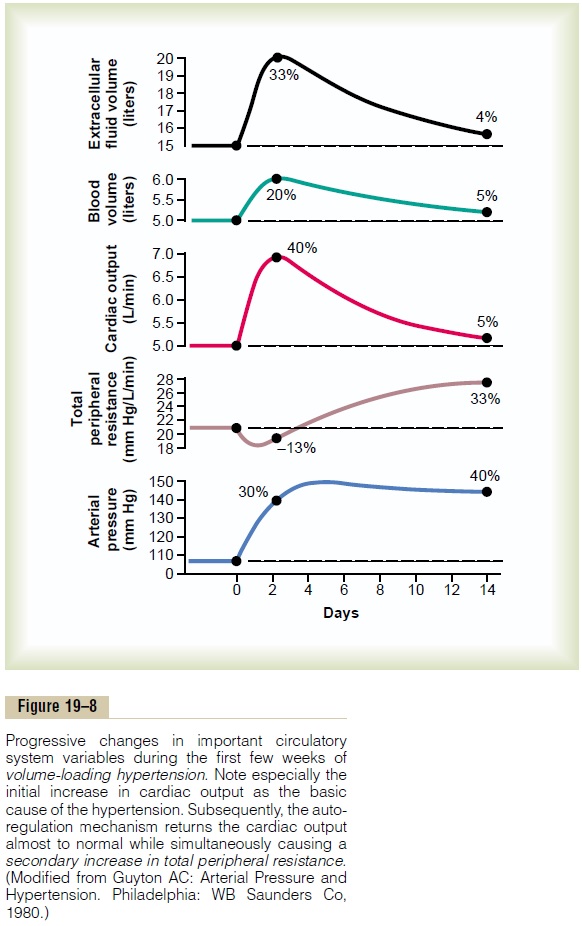
point, the intake of salt and water was increased to about six times normal and kept at this high intake thereafter. The acute effect was to increase extracellu-lar fluid volume, blood volume, and cardiac output to 20 to 40 per cent above normal. Simultaneously, the arterial pressure began to rise but not nearly so much at first as did the fluid volumes and cardiac output. The reason for this slower rise in pressure can be discerned by studying the total peripheral resistance curve, which shows an initial decrease in total peripheral resistance. This decrease was caused by the baroreceptor mechanism, which tried to prevent the rise in pressure. However, after 2 to 4 days, the baroreceptors adapted (reset) and were no longer able to prevent the rise in pressure. At this time, the arte-rial pressure had risen almost to its full height because of the increase in cardiac output, even though the total peripheral resistance was still almost at the normal level.
After these early acute changes in the circulatory variables had occurred, more prolonged secondary changes occurred during the next few weeks. Espe-cially important was a progressive increase in totalperipheral resistance, while at the same time the cardiac output decreased almost all the way back to normal,mainly as a result of the long-term blood flow autoreg-ulation mechanism that is discussed in detail earlier. That is, after the cardiac output had risen to a high level and had initi-ated the hypertension, the excess blood flow through the tissues then caused progressive constriction of the local arterioles, thus returning the local blood flows in all the body tissues and also the cardiac output almost all the way back to normal, while simultane-ously causing a secondary increase in total peripheralresistance.
Note, too, that the extracellular fluid volume and blood volume returned almost all the way back to normal along with the decrease in cardiac output. This resulted from two factors: First, the increase in arteri-olar resistance decreased the capillary pressure, which allowed the fluid in the tissue spaces to be absorbed back into the blood. Second, the elevated arterial pressure now caused the kidneys to excrete the excess volume of fluid that had initially accumulated in the body.
Last, let us take stock of the final state of the circu-lation several weeks after the initial onset of volume loading. We find the following effects:
1. Hypertension
2. Marked increase in total peripheral resistance
3. Almost complete return of the extracellular fluid volume, blood volume, and cardiac output back to normal
Therefore, we can divide volume-loading hyperten-sion into two separate sequential stages:The first stage results from increased fluid volume causing increased cardiac output. This increase in cardiac output causes the hypertension. The second stage in volume-loading hypertension is characterized by high blood pressure and high total peripheral resistance but return of the cardiac output so near to normal that the usual meas-uring techniques frequently cannot detect an abnor-mally elevated cardiac output.
Thus, the increased total peripheral resistance in volume-loading hypertension occurs after the hyper-tension has developed and, therefore, is secondary to the hypertension rather than being the cause of the hypertension.
Volume-Loading Hypertension in Patients Who Have No Kidneys but Are Being Maintained on an Artificial Kidney
When a patient is maintained on an artificial kidney, it is especially important to keep the patient’s body fluid volume at a normal level—that is, it is important to remove an appropriate amount of water and salt each time the patient is dialyzed. If this is not done and extracellular fluid volume is allowed to increase, hypertension almost invariably develops in exactly the same way as shown in Figure 19–8. That is, the cardiac output increases at first and causes hypertension. Then the autoregulation mechanism returns the cardiac output back toward normal while causing a secondary increase in total peripheral resistance. Therefore, in the end, the hypertension is a high peripheral resist-ance type of hypertension.
Hypertension Caused by Primary Aldosteronism
Another type of volume-loading hypertension is caused by excess aldosterone in the body or, occa-sionally, by excesses of other types of steroids. A small tumor in one of the adrenal glands occasionally secretes large quantities of aldosterone, which is the condition called “primary aldosteronism.”, aldosterone increases the rate of reabsorption of salt and water by the tubules of the kidneys, thereby reducing the loss of these in the urine while at the same time causing an increase in blood volume and extracellular fluid volume. Conse-quently, hypertension occurs. And, if salt intake is increased at the same time, the hypertension becomes even greater. Furthermore, if the condition persists for months or years, the excess arterial pressure often causes pathological changes in the kidneys that make the kidneys retain even more salt and water in addi-tion to that caused directly by the aldosterone. There-fore, the hypertension often finally becomes lethally severe.
Here again, in the early stages of this type of hyper-tension, the cardiac output is increased, but in later stages, the cardiac output generally returns almost to normal while the total peripheral resistance becomes secondarily elevated.
Related Topics