Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Chronic Pain Management
Cervicothoracic (Stellate) Block
Cervicothoracic (Stellate) Block
A. Indications
This block is often used for patients with
head, neck, arm, and upper chest pain. It is commonly referred to as a stellate
block but usually blocks the upper thoracic as well as all cervical ganglia.
Injection of larger volumes of anesthetic often extends the block to the T5
ganglia. Stellate blocks may also be used for vasospastic disorders of the
upper extremity.
B. Anatomy
Sympathetic innervation of the head, neck,
and most of the arm is derived from four cervical gan-glia, the largest being
the stellate ganglion. The latter usually represents a fusion of the lower
cervical and first thoracic ganglia. Some sympathetic innervation of the arm
(T1) as well as innervation of all of the thoracic viscera derives from the
five upper thoracic ganglia. The sympathetic supply to the arm in some persons
may also originate from T2–T3 via ana-tomically distinct nerves (Kuntz’s
nerves) that join the brachial plexus high in the axilla. These nerves may be
missed by a stellate block but not an axil-lary block. The point of injection
is at the level of the stellate, which lies posterior to the origin of the
vertebral artery from the subclavian artery, anterior to the longus colli
muscle and the first rib, antero-lateral to the prevertebral fascia, and medial
to the scalene muscles.
C. Technique
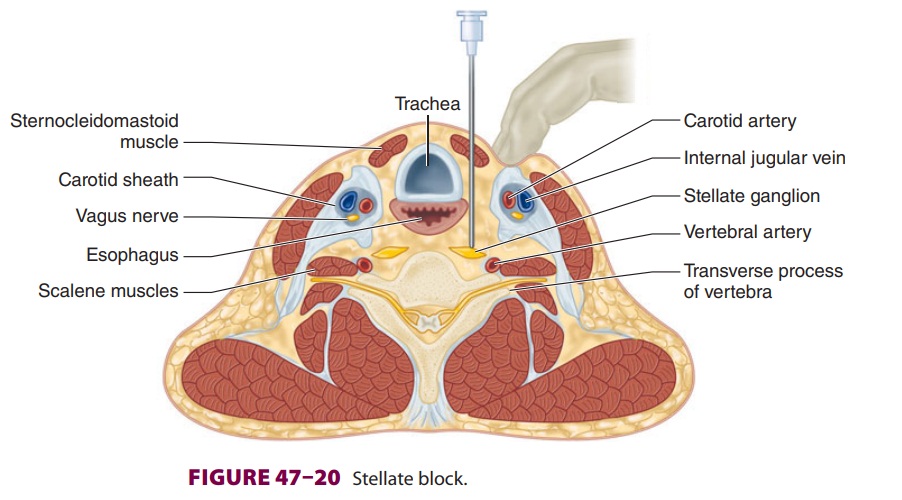
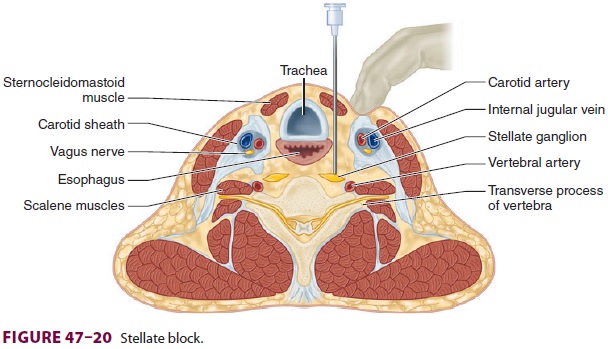
The paratracheal technique is most commonly
used (Figure 47–20), although an oblique
or posterior approach may also be taken. With the patient’s head extended, a 4-
to 5-cm 22-gauge needle is inserted at the medial edge of the
sternocleidomastoid mus-cle just below the level of the cricoid cartilage at
the level of the transverse process of C6 (Chassaignac’s tubercle) or C7 (3–5
cm above the clavicle). The non-operative hand should be used to retract the
muscle together with the carotid sheath prior to needle insertion. The needle
is advanced to the transverse process and withdrawn 2–3 mm prior to injection.
Aspiration must be carried out in two planes before1-mL test dose is used to
exclude unintentional intravascular injection into the vertebral or subcla-vian
arteries or subarachnoid injection into a dural sleeve. A total of 5–10 mL of
local anesthetic may be injected. Although this procedure is often per-formed
under fluoroscopy, ultrasound may also be used to visualize the anatomy and
decrease the risk of inadvertent intravascular injection.
Correct placement of the needle is usually
fol-lowed promptly by an increase in the skin tempera-ture of the ipsilateral
arm and the onset of Horner’s syndrome. The latter consists of ipsilateral
ptosis, meiosis, enophthalmos, nasal congestion, and anhy-drosis of the neck
and face. This may be consideredside effect of the block rather than a
complication.
D. Complications
In addition to intravascular and subarach-noid injection, other complications of stellateblock include hematoma, pneumothorax, epidural anesthesia, brachial plexus block, hoarseness due to blockade of the recurrent laryngeal nerve, and, rarely, osteomyelitis or mediastinitis following esophageal puncture, particularly if a left-sided approach is taken. The posterior approach may have the highest incidence of pneumothorax.
Related Topics