Chapter: Obstetrics and Gynecology: Cervical Neoplasia and Carcinoma
Cervical Carcinoma
CERVICAL CARCINOMA
Between 1950 and 1992, the death
rate from cervical can-cer declined by 74%. The main reason for this steep
decrease is the increasing use of the Pap test for cervical cancer screening.
The death rate continues to decline by approximately 4% per year. Despite the
progress made in early detection and treatment, approximately 11,000 new cases
of invasive cervical carcinoma are diagnosed annually with 3870 deaths.
The average age at diagnosis for
invasive cervical can-cer is approximately 50 years, although the disease may
occur in the very young as well as the very old patient. In studies following
patients with advanced CIN, this precur-sor lesion precedes invasive carcinoma
by approximately 10 years. In some patients, however, this time of progres-sion
may be considerably less.
The etiology of cervical cancer is HPV in more than 90% of the cases. The two major histologic types of inva-sive cervical carcinomas are squamous cell carcinomas and adenocarcinomas. Squamous cell carcinomas comprise 80% of cases, and adenocarcinoma or adenosquamous car-cinoma comprise approximately 15%. The remaining cases are made up of various rare histologies that behave differ-ently from squamous cell cancer and adenocarcinoma.
Clinical Evaluation
The signs and symptoms of early
cervical carcinoma are variable and nonspecific, including watery vaginal
dis-charge, intermittent spotting, and postcoital bleeding. Often the symptoms
go unrecognized by the patient. Because of the accessibility of the cervix,
accurate diagno-sis often can be made with cytologic screening,
colpo-scopically directed biopsy, or biopsy of a gross or palpable lesion. In
cases of suspected microinvasion and early-stage cervical carcinoma, conization
of the cervix is indi-cated to evaluate the possibility of invasion or to
define the depth and extent of microinvasion. CKC provides the most accurate
evaluation of the margins.
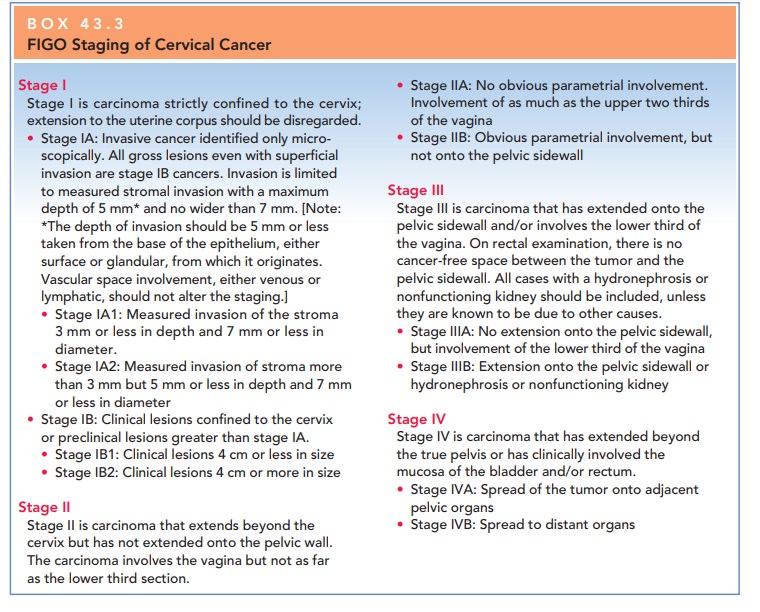
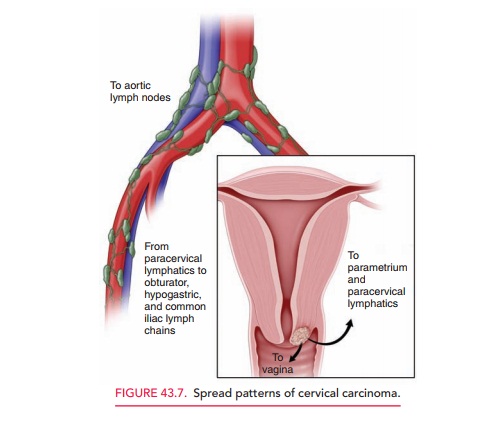
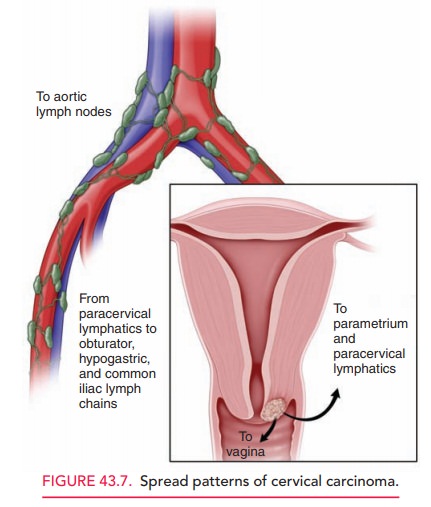
Staging is based on the
International Federation of Gynecology and Obstetrics (FIGO) Staging
Classification (Box 43.3). This classification is based both on the histo-logic
assessment of the tumor sample and on physical and laboratory examination to
ascertain the extent of disease. It is useful because of the predictable manner
in which cervical carcinoma spreads by direct invasion and by lym-phatic
metastasis (Fig. 43.7). Careful clinical examination should be performed on all
patients. Examinations should be conducted by experienced examiners, and may be
per-formed under anesthesia. Pretreatment evaluation of women with cervical
carcinoma often can be helpful if provided by an obstetrician–gynecologist with
advanced surgical training, experience, and demonstrated compe-tence, such as a
gynecologic oncologist. Various optional examinations, such as ultrasonography,
computed tomog-raphy (CT), magnetic resonance imaging (MRI), lym-phangiography,
laparoscopy, and fine-needle aspiration, are valuable for treatment planning
and to help define the extent of tumor growth, especially in patients with
locally advanced disease (i.e., stage IIb or more advanced). Sur-gical findings
provide extremely accurate information about the extent of disease and will
guide treatment plans, but will not change the results of clinical staging.
Management
The clinician should be familiar with the options for treat-ing women with both early and advanced cervical cancer and should facilitate referrals for this treatment. Surgery or radiation therapy may be options for treatment, depending on the stage and size of the lesion:
·
Patients with squamous cell
cancers and those with ade-nocarcinomas should be managed similarly, except for
those with microinvasive disease. Criteria for micro-invasive adenocarcinomas
have not been established.
·
For stage Ia1, microinvasive
squamous carcinoma of the cervix, treatment with conization of the cervix or
sim-ple extrafascial hysterectomy may be considered.
·
Stage Ia2, invasive squamous
carcinoma of the cervix, should be treated with radical hysterectomy with lymph
node dissection or radiation therapy, depending on clin-ical circumstances.
·
Stage Ib1 should be distinguished
from stage Ib2 carci-noma of the cervix, because the distinction predictsnodal
involvement and overall survival and may there-fore affect treatment and
outcome.
· For stage
Ib and selected IIa carcinomas of the cervix, either radical hysterectomy and
lymph node dissection or radiation therapy with cisplatin-based chemotherapy
should be considered. Adjuvant radiation therapy may be required in those
treated surgically, based on pathologic risk factors, especially in those with
stage Ib2 carcinoma.
· Stage IIb
and greater should be treated with external-beam and brachytherapy radiation
and concurrent cisplatin-based chemotherapy.
Brachytherapy delivers radiation close to the affected organ or structure. Both high- and low-dose brachytherapy are used to treat cervical cancer. The brachytherapy radiation is delivered using special apparatuses known as tandem and ovoid devices placed through the cervix into the uterus and at the apices of the vagina. The external beam radiation is applied primarily along the paths of lymphatic extension of cervical carcinoma in the pelvis.
The structures close to the
cervix, such as the bladder and distal colon, tolerate radiation relatively
well. Radiation therapy doses are calculated by individual-patient needs to
maximize radiation to the tumor sites and potential spread areas, while
minimizing the amount of radiation to adjacent uninvolved tissues.
Complications of radiation therapy include radiation cystitis and proctitis, which
are usually relatively easy to manage. Other more unusual complica-tions
include intestinal or vaginal fistulae, small bowel obstruction, or
difficult-to-manage hemorrhagic proctitis or cystitis. Tissue damage and
fibrosis incurred by radiation therapy progresses over many years, and these
effects may complicate long-term management.
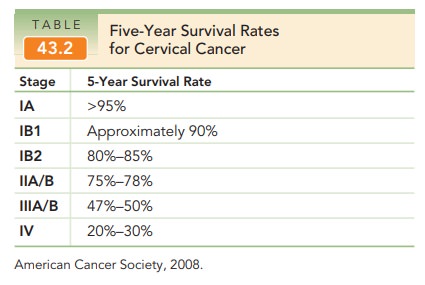
Following treatment for cervical
carcinoma, patients should be monitored regularly, for example, with
thrice-yearly follow-up examinations for the first 2 years and twice-yearly
visits subsequently to year 5, with Pap tests annually and chest x-rays
annually for up to 5 years. The five-year survival rates for cervical cancer
are listed in Table 43.2.
Treatment for recurrent disease is associated with poor cure rates. Most chemotherapeutic protocols have only limited usefulness and are reserved for palliative efforts. Likewise, specific “spot” radiation to areas of recurrence also provides only limited benefit.
Occasional patients with central recurrence (i.e.,
recurrence of disease in the upper vagina or the residual cervix and uterus in
radiation patients) may benefit from ultraradical surgery with partial or total
pelvic exenteration. These candidates are few, but when properly selected, may
benefit from this aggressive therapy.
Related Topics