Chapter: Medical Physiology: Muscle Blood Flow and Cardiac Output During Exercise; the Coronary Circulation and schemic Heart Disease
Causes of Death After Acute Coronary Occlusion
Causes of Death After Acute Coronary Occlusion
The most common causes of death after acute myocardial infarction are (1) decreased cardiac output;(2) damming of blood in the pulmonary blood vessels and then death resulting from pulmonary edema; (3) fibrillation of the heart; and, occasionally, (4) rupture of the heart.
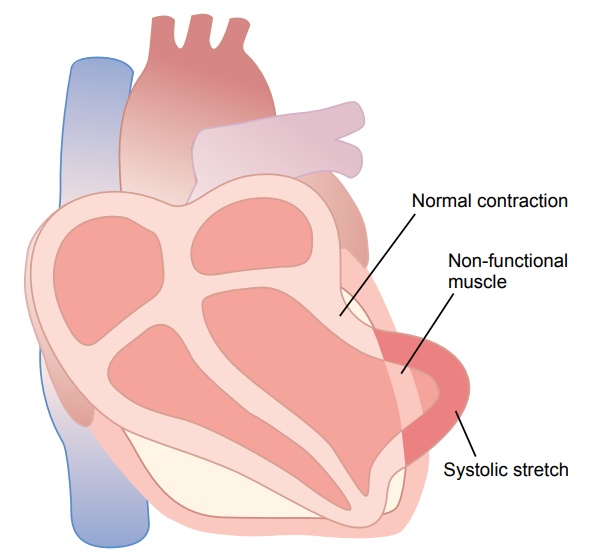
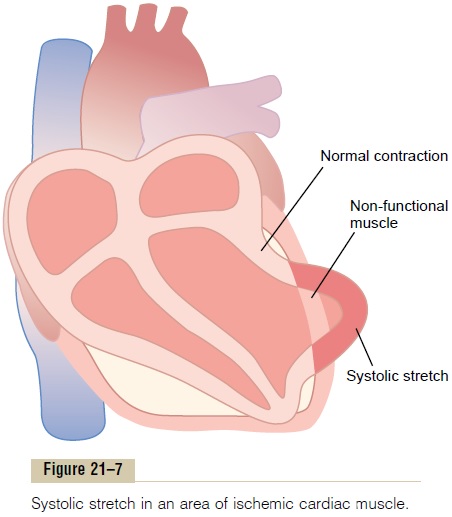
DecreasedCardiacOutput—SystolicStretchandCardiac Shock. When some of the cardiac muscle fibers are notfunctioning and others are too weak to contract with great force, the overall pumping ability of the affected ventricle is proportionately depressed. Indeed, the overall pumping strength of the infarcted heart is often decreased more than one might expect because of a phenomenon called systolic stretch, shown in Figure 21–7. That is, when the normal portions of the ventric-ular muscle contract, the ischemic portion of the muscle, whether this be dead or simply nonfunctional, instead of contracting is forced outward by the pres-sure that develops inside the ventricle. Therefore much of the pumping force of the ventricle is dissi-pated by bulging of the area of nonfunctional cardiac muscle.
When the heart becomes incapable of contracting with sufficient force to pump enough blood into the peripheral arterial tree, cardiac failure and death of peripheral tissues ensue as a result of peripheralischemia. This condition is called coronary shock, car-diogenic shock, cardiac shock, or low cardiac output failure. It is discussed more fully in the next.Cardiac shock almost always occurs when more than 40 per cent of the left ventricle is infarcted. And death occurs in about 85 per cent of patients once they develop cardiac shock.
Damming of Blood in the Body’s Venous System. When theheart is not pumping blood forward, it must be damming blood in the atria and in the blood vessels of the lungs or in the systemic circulation. This leads to increased capillary pressures, particularly in the lungs.
This damming of blood in the veins often causes little difficulty during the first few hours after myocar-dial infarction. Instead, symptoms develop a few days later for the following reason: The acutely diminished cardiac output leads to diminished blood flow to the kidneys. The kidneys fail to excrete enough urine. This adds progressively to the total blood volume and, therefore, leads tocongestive symptoms. Consequently, many patients who seemingly are getting along well during the first few days after onset of heart failure will suddenly develop acute pulmonary edema and often will die within a few hours after appearance of the initial pulmonary symptoms.
Fibrillation of the Ventricles After Myocardial Infarction.
Many people who die of coronary occlusion die because of sudden ventricular fibrillation. The ten-dency to develop fibrillation is especially great after a large infarction, but fibrillation can sometimes occur after small occlusions as well. Indeed, some patients with chronic coronary insufficiency die suddenly fromfibrillation without any acute infarction.
There are two especially dangerous periods after coronary infarction during which fibrillation is most likely to occur. The first is during the first 10 minutes after the infarction occurs. Then there is a short period of relative safety, followed by a secondary period of cardiac irritability beginning 1 hour or so later and lasting for another few hours. Fibrillation can also occur many days after the infarct but less likely so.
At least four factors enter into the tendency for the heart to fibrillate:
1. Acute loss of blood supply to the cardiac muscle causes rapid depletion of potassium from the ischemic musculature. This also increases the potassium concentration in the extracellular fluids surrounding the cardiac muscle fibers. Experiments in which potassium has been injected into the coronary system have demonstrated that an elevated extracellular potassium concentration increases the irritability of the cardiac musculature and, therefore, its likelihood of fibrillating.
2. Ischemia of the muscle causes an “injury current,”. That is, the ischemic musculature often cannot completely repolarize its membranes after a heart beat, so that the external surface of this muscle remains negative with respect to normal cardiac muscle membrane potential elsewhere in the heart. Therefore, electric current flows from this ischemic area of the heart to the normal area and can elicit abnormal impulses that can cause fibrillation.
3. Powerful sympathetic reflexes often develop aftermassive infarction, principally because the heart does not pump an adequate volume of blood into the arterial tree. The sympathetic stimulation also increases irritability of the cardiac muscle and thereby predisposes to fibrillation.
4. Cardiac muscle weakness caused by themyocardial infarction often causes the ventricle todilate excessively. This increases the pathway length for impulse conduction in the heart and frequentlycauses abnormal conduction pathways all the wayaround the infarcted area of the cardiac muscle.Both of these effects predispose to development of circus movements because, excess prolongation of conduction pathways in the ventricles allows impulses to re-enter muscle that is already recovering from refractoriness, thereby initiating a “circus movement” cycle of new excitation and causing the process to continue on and on.
Rupture of the Infarcted Area. During the first day or soafter an acute infarct, there is little danger of rupture of the ischemic portion of the heart, but a few days later, the dead muscle fibers begin to degenerate, and the heart wall becomes stretched very thin. When this happens, the dead muscle bulges outward severely with each heart contraction, and this systolic stretch becomes greater and greater until finally the heart rup-tures. In fact, one of the means used in assessing progress of severe myocardial infarction is to record by cardiac imaging (i.e., x-rays) whether the degree of systolic stretch is worsening.
When a ventricle does rupture, loss of blood into the pericardial space causes rapid development of cardiactamponade—that is, compression of the heart from theoutside by blood collecting in the pericardial cavity. Because of this compression of the heart, blood cannot flow into the right atrium, and the patient dies of sud-denly decreased cardiac output.
Related Topics