Chapter: Psychiatric Mental Health Nursing : Eating Disorders
Categories of Eating Disorders and Related Disorders
CATEGORIES OF EATING DISORDERS
AND RELATED DISORDERS
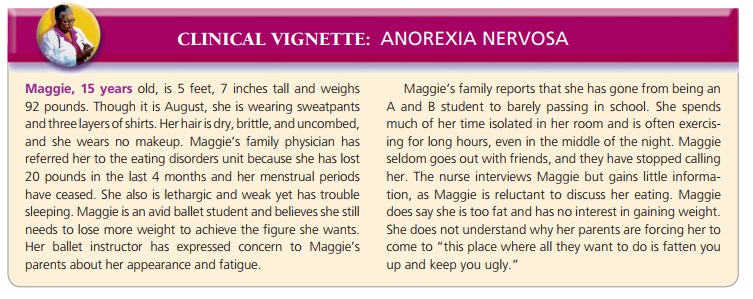
Anorexia nervosa is a life-threatening eating
disorder characterized by the
client’s refusal or inability to maintain a minimally normal body weight,
intense fear of gaining weight or becoming fat, significantly disturbed
perception of the shape or size of the body, and steadfast inability or refusal
to acknowledge the seriousness of the problem or even that one exists (APA,
2000). Clients with anorexia have a body weight that is 85% or less of that
expected for their age and height, have experienced amenorrhea for at least
three consecutive cycles, and have a preoccupation with food and food-related activities.
Clients with anorexia nervosa can be classified into two subgroups
depending on how they control their weight. Clients with the restricting
subtype lose weight primarily through dieting, fasting, or excessive
exercising. Those with the binge eating and purging subtype engage regu-larly
in binge eating followed by purging. Binge
eating means consuming a large amount of food (far greater than most people
eat at one time) in a discrete period of usually 2 hours or less. Purging involves compensatory behaviors
designed to eliminate food by means of self-induced vom-iting or misuse of
laxatives, enemas, and diuretics. Some clients with anorexia do not binge but
still engage in purg-ing behaviors after ingesting small amounts of food.
Clients with anorexia become totally absorbed in their quest for
weight loss and thinness. The term anorexia
is actually a misnomer: These clients do not lose their appe-tites. They still
experience hunger but ignore it and signs of physical weakness and fatigue;
they often believe that if they eat anything, they will not be able to stop
eating and will become fat. Clients with anorexia often are preoccu-pied with
food-related activities such as grocery shopping, collecting recipes or
cookbooks, counting calories, creat-ing fat-free meals, and cooking family
meals. They also may engage in unusual or ritualistic food behaviors such as
refusing to eat around others, cutting food into minute pieces, or not allowing
the food they eat to touch their lips. These behaviors increase their sense of
control. Excessive exercise is common; it may occupy several hours a day.
Bulimia nervosa, often simply called
bulimia, is an eat-ing disorder characterized by recurrent episodes (at least
twice a week for 3 months) of binge eating followed by inappropriate
compensatory behaviors to avoid weight gain, such as purging, fasting, or
excessively exercising (APA, 2000). The amount of food consumed during a binge
episode is much larger than a person would normally eat. The client often
engages in binge eating secretly. Between binges, the client may eat
low-calorie foods or fast. Binging or purging episodes are often pre-cipitated
by strong emotions and followed by guilt, remorse, shame, or self-contempt.
The weight of clients with bulimia usually is in the nor-mal range,
although some clients are overweight or under-weight. Recurrent vomiting
destroys tooth enamel, and incidence of dental caries and ragged or chipped
teeth increases in these clients. Dentists are often the first health care
professionals to identify clients with bulimia.
Related eating disorders usually first diagnosed in infancy and
childhood include rumination disorder,
pica, and feeding disorder . Common elements in clients with these disorders
are family dysfunction and parent–child conflicts.
Binge eating disorder is listed as a research
category in the DSM-IV-TR (APA,
2000); it is being investigated to deter-mine its classification as a mental
disorder. The essential features are recurrent episodes of binge eating; no
regular use of inappropriate compensatory behaviors, such as purg-ing or
excessive exercise or abuse of laxatives; guilt, shame, and disgust about
eating behaviors; and marked psycho-logic distress. Binge eating disorder
frequently affects people over age 35, and it occurs often in men (Yager,
2008). Indi-viduals are more likely to be overweight or obese, over-weight as
children, and teased about their weight at an early age. Thirty-five percent
reported that binge eating preceded dieting; 65% reported dieting before binge
eating.
Night eating syndrome is characterized by morning anorexia, evening hyperphagia
(consuming 50% of daily calories after the last evening meal), and nighttime
awak-enings (at least once a night) to consume snacks. It is asso-ciated with
life stress, low self-esteem, anxiety, depression, and adverse reactions to
weight loss. Most people with night eating syndrome are obese (Stunkard,
Allison, & Lundgren, 2008). Treatment with SSRI antidepressants has shown
positive effects.
![]()
![]() Comorbid psychiatric disorders are common in
clients with anorexia nervosa and bulimia nervosa. Mood disor-ders, anxiety
disorders, and substance abuse/dependence are frequently seen in clients with
eating disorders. Of those, depression and obsessive–compulsive disorder are
most common (Anderson & Yager, 2005). Anorexia and bulimia are both
characterized by perfectionism, obsessive–compulsiveness, neuroticism, negative
emo-tionality, harm avoidance, low self-directedness, low cooperativeness, and
traits associated with avoidant per-sonality disorder. In addition, clients
with bulimia may also exhibit high impulsivity, sensation seeking, novelty
seeking, and traits associated with borderline personality disorder (Thompson,
2009). Eating disorders often are linked to a history of sexual abuse,
especially if the abuse occurred before puberty (Pike et al., 2008). Such a
history may be a factor contributing to problems with intimacy, sexual
attractiveness, and low interest in sexual activity. Clients with eating
disorders and a history of sexual abuse also have higher levels of depression
and anxiety, lower self-esteem, more interpersonal problems, and more severe
obsessive–compulsive symptoms (Carter et al., 2006). Whether sexual abuse has a
cause-and- effect relationship with the development of eating disorders,
however, remains unclear.
Comorbid psychiatric disorders are common in
clients with anorexia nervosa and bulimia nervosa. Mood disor-ders, anxiety
disorders, and substance abuse/dependence are frequently seen in clients with
eating disorders. Of those, depression and obsessive–compulsive disorder are
most common (Anderson & Yager, 2005). Anorexia and bulimia are both
characterized by perfectionism, obsessive–compulsiveness, neuroticism, negative
emo-tionality, harm avoidance, low self-directedness, low cooperativeness, and
traits associated with avoidant per-sonality disorder. In addition, clients
with bulimia may also exhibit high impulsivity, sensation seeking, novelty
seeking, and traits associated with borderline personality disorder (Thompson,
2009). Eating disorders often are linked to a history of sexual abuse,
especially if the abuse occurred before puberty (Pike et al., 2008). Such a
history may be a factor contributing to problems with intimacy, sexual
attractiveness, and low interest in sexual activity. Clients with eating
disorders and a history of sexual abuse also have higher levels of depression
and anxiety, lower self-esteem, more interpersonal problems, and more severe
obsessive–compulsive symptoms (Carter et al., 2006). Whether sexual abuse has a
cause-and- effect relationship with the development of eating disorders,
however, remains unclear.
Related Topics