Chapter: Case Study in Obstetrics and Gynaecology: General Obstetrics
Case Study Reports: Postpartum Pyrexia
POSTPARTUM PYREXIA
History
A
29-year-old woman presents with a fever.
She had a Caesarean section
3 weeks ago
and was recovering well until 2 days ago when she became very cold and shivery at night. She has
been unable to keep herself
warm despite several
blankets and has reduced appetite, nausea, vomiting and lethargy. She is breast-feeding and has had
very sore nipples
since the birth but
feels this is normal and
has been using
camomile ointment to soothe them. In the last 24 h she has noticed
the left breast
has become sore and red.
She
has mild lower
abdominal pain at the site of the Caesarean section
wound. She no longer has vaginal bleeding
but has a moderate brown
discharge with an odour which
she says is improving. Bowel habit is normal and
she has no urinary symptoms.
Examination
On
examination the woman is wearing
a jersey and jacket, with a blanket
over her. Her temperature is 38.6°C. Blood
pressure is 120/64
mmHg and heart
rate 106/min. The chest
is clear and heart sounds
are normal. The right breast
is normal but there is a well- demarcated area of redness
over the superiolateral aspect of the left breast,
which is ten- der and hot to touch.
The
uterus is firm and is non-tender, just palpable above
the symphysis pubis.
There is no leg
swelling.
Questions
·
How would you interpret the investigations?
·
What is the likely diagnosis and differential diagnosis?
·
How
would you investigate and manage this woman?
ANSWER
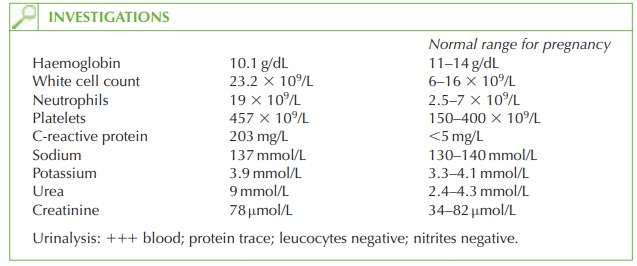
The
blood and protein
on urinalysis are
likely to be due to contamination from
persisting vaginal discharge (lochia), but there is no evidence
of urinary tract
infection (no leuco- cytes or nitrites).
The
haemoglobin is slightly
low, which can occur
with sepsis but is also common after pregnancy and delivery. The leucocytosis with neutrophilia and raised C-reactive protein suggests a significant bacterial septic process. Urea is raised
while creatinine and
potas- sium are normal,
suggesting dehydration secondary to sepsis, pyrexia
and vomiting.
Diagnosis
The
diagnosis is mastitis
(a localized infection
within the breast tissue). This occurs in 5 per cent of lactating women. The pathophysiology probably involves colonization of the breast ducts
by bacteria through the cracked nipples, causing localized inflammation and
obstruction of the duct with subsequent retention of milk, and infection. The commonest
organism is staphylococcus from the
skin. The differential diagnosis is of a breast
abscess which would be palpated as a fluctuant mass in the breast.
Investigation
Blood cultures and a swab from the breast
milk or nipple
are necessary. In cases of diag-
nostic doubt, an ultrasound scan can differentiate mastitis from an abscess.
Management
The
woman should be admitted for intravenous antibiotics and fluids, regular
paraceta- mol, analgesia and anti-emetics as necessary. Until
cultures are available, flucloxacillin should be commenced with consultation with
a microbiologist if some improvement is not seen within
24 h.
She
should be encouraged to continue breast-feeding. If this is too painful
she should express milk in order
to try to unblock
the duct. If an abscess
is diagnosed then needle
aspir- ation under
local anaesthetic is preferred to formal incision
and drainage in most cases.
Related Topics