Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Cardiopulmonary Resuscitation
Cardiopulmonary Resuscitation: Circulation
CIRCULATION
Circulation
takes precedence over
airway and breathing in a cardiac
arrest situation. In this scenario, as previously noted, chest compressions
should begin prior to the initial breaths. Subse-quent actions to assess
circulation may then vary depending on whether the responder is a lay person or
health care provider. Although lay rescuers should assume that an unresponsive patient is in cardiac arrest and need not check pulse;
health care provid-ers should assess for presence or absence of a pulse.
After successful delivery of two initial
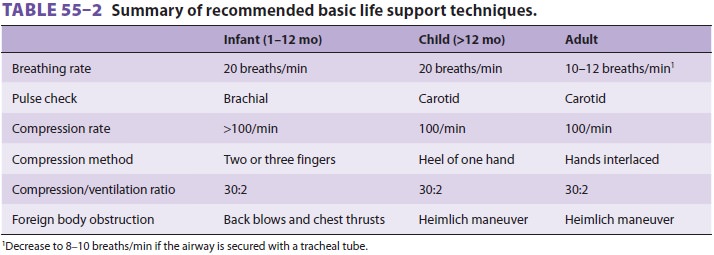
breaths (each 2 s in duration), circulation is rapidly assessed. If the patient
has an adequate pulse (carotid artery in an adult or child, brachial or femoral
artery in an infant) or blood pressure, breathing is continued at 10–12
breaths/min for an adult or a child older than 8 years, and 20 breaths/min for
an infant or a child younger than 8 years of age (Table 55–2). If the patient
is pulseless or severely hypotensive, the circulatory system must be supported
by a combi-nation of external chest compressions, intravenous drug
administration, and defibrillation when appro-priate. Initiation of chest
compressions is mandated by the inadequacy of peripheral perfusion, and drug
choices and defibrillation energy levels often depend on electrocardiographic diagnosis
of arrhythmias.
External Chest Compression
Chest compressions force blood to f low
either by increasing intrathoracic pressure (thoracic pump) or by directly
compressing the heart (cardiac pump). During CPR of short duration, the blood
flow is cre-ated more by the cardiac pump mechanism; as CPR continues, the
heart becomes less compliant and the thoracic pump mechanism becomes more
important. As important as the rate and force of compression are for
maintaining blood flow, eff ective perfusion of the heart and brain is best
achieved when chest compression consumes 50% of the duty cycle, with the
remaining 50% devoted to the relaxation phase (allowing blood return into the
chest and heart).
To perform chest compressions in the
unre-sponsive or pulseless patient, the xiphoid process is located and the heel
of the rescuer’s hand is placed over the lower half of the sternum. The other
hand is placed over the hand on the sternum with the fingers either interlaced
or extended, but off the chest. The rescuer’s shoulders should be positioned
directly over the hands with the elbows locked into position and arms extended,
so that the weight of the upper body is used for compressions. With a straight
downward thrust, the sternum is depressed 1½–2 in. (4–5 cm) in adults, 1–1½ in.
(2–4 cm) in children, and then allowed to return to its normal position. For an
infant, compressions ½–1 in. (1½–2½ cm) in depth are made with the middle and
ring fingers on the sternum one finger-breadth below the nipple line. Compression
and release times should be equal.
Whether adult resuscitation is performed by a
single rescuer or by two rescuers, two breathsare
administered every 30 compressions (30:2), allowing 3–4 s for the two breaths.
The cardiac com-pression rate should be 100/min regardless of the number of
rescuers. A slightly higher compression rate of more than 100/min is suggested
for infants, with two breaths delivered every 30 compressions.
Assessing the Adequacy of Chest Compressions
Cardiac
output can be estimated by monitoring end-tidal CO 2 (Petco2>10 mm Hg, Scvo2>30%) or arterial pulsations (with an
arterial diastolic relax-ation pressure >20 mm Hg). Arterial pulsations
dur-ing resuscitation are not a good measure of adequate chest compression;
however, spontaneous arterial pulsations are an indicator of ROSC. There is new
emphasis in the 2010 guidelines on physiological parameters, such as Petco2,
Scvo2, and diastolic arterial pressure, to assess the adequacy of
chest compressions.
1. Petco2—In an intubatedpatient,aPetco2greaterthan 10 mm Hg indicates good-quality chest com-pressions; a Petco2 less than 10 mm Hg has been shown to be a predictor of poor outcomes of CPR (decreased chance of ROSC). A transient increase in Petco2 may be seen with administration of sodium bicarbonate; however, an abrupt and sustained riseof Petco2 is an indicator of ROSC.
2. Coronary perfusion pressure (CPP)—Thisis thedifference between the
aortic diastolic pressure and the right atrial diastolic pressure. Arterial
diastolic pressure in the radial, brachial, or femoral artery is good indicator
of CPP. Arterial diastolic pressure greater than 20 mm Hg is an indicator of
adequate chest compressions.
3. Scvo2—AnScvo2less than 30%inthe
jugular veinis associated with poor outcomes. If the Scvo2 is less
than 30%, attempts to improve the quality of CPR, either by improving the
quality of compressions or through administration of medications, should be
considered.
Related Topics