Chapter: Essentials of Psychiatry: Eating Disorders
Bulimia Nervosa
Bulimia
Nervosa
Definition
The
salient behavioral disturbance of bulimia nervosa is the occurrence of episodes
of binge-eating. During these episodes, the individual consumes an amount of
food that is unusually large considering the circumstances under which it was
eaten. Although this is a useful definition and conceptu-ally reasonably clear,
it can be operationally difficult to distin-guish normal overeating from a
small episode of binge-eating. Indeed, the available data do not suggest that
there is a sharp dividing line between the size of binge-eating episodes and
the size of other meals. On the other hand, while the border between normal and
abnormal eating may not be a sharp one, both patients’ reports and laboratory
studies of eating behavior clearly indicate that, when binge-eating, patients
with bulimia nervosa do indeed consume larger than normal amounts of food.
Episodes
of binge-eating are associated, by definition, with a sense of loss of control.
Once the eating has begun, the in-dividual feels unable to stop until an
excessive amount has been consumed. This loss of control is only subjective, in
that most individuals with bulimia nervosa will abruptly stop eating in the
midst of a binge episode if interrupted, for example, by the unex-pected
arrival of a roommate.
After overeating, individuals with bulimia nervosa en-gage in some form of inappropriate behavior in an attempt to avoid weight gain. Most patients who present to eating disorders clinics with this syndrome report self-induced vomiting or the abuse of laxatives. Other methods include misusing diuretics, fasting for long periods and exercising extensively after eating binges.
The
DSM-IV-TR criteria require that the overeating epi-sodes and the compensatory
behaviors both occur at least twice a week for 3 months to merit a diagnosis of
bulimia nervosa. This criterion, although useful in preventing the diagnostic
label from being applied to individuals who only rarely have difficulty with
binge-eating, is clearly an arbitrary one.
Criterion
D in the DSM-IV-TR definition of bulimia ner-vosa requires that individuals
with bulimia nervosa exhibit an over concern with body shape and weight. That
is, they tend to base much of their self-esteem on how much they weigh and how
slim they look.
Finally,
in the DSM-IV-TR nomenclature, the diagnosis of bulimia nervosa is not given to
individuals with anorexia ner-vosa. Individuals with anorexia nervosa who
recurrently engage in binge-eating or purging behavior should be given the
diag-nosis of anorexia nervosa, binge-eating/purging subtype, rather than an
additional diagnosis of bulimia nervosa.
In
DSM-IV-TR, a subtyping scheme was introduced for bulimia nervosa in which
patients are classed as having either the purging or the nonpurging type of
bulimia nervosa. This scheme was introduced for several reasons. First, those
indi-viduals who purge are at greater risk for the development of fluid and
electrolyte disturbances such as hypokalemia. Sec-ondly, data suggest that
individuals with the nonpurging type of bulimia nervosa weigh more and have
less psychiatric illness compared with those with the purging type. Finally,
most of the published literature on the treatment of bulimia nervosa has been
based on studies of individuals with the purging type of this disorder.
Epidemiology
Soon
after bulimia nervosa was recognized as a distinct dis-order, surveys indicated
that many young women reported problems with binge-eating, and it was suggested
that the syn-drome of bulimia nervosa was occurring in epidemic propor-tions.
Later careful studies have found that although binge-eating is frequent, the
full-blown disorder of bulimia nervosa is much less common, probably affecting
1 to 2% of young women in the USA. Although sufficient research data do not
exist to pinpoint specific epidemiological trends in the occur-rence of bulimia
nervosa, research suggests that women born after 1960 have a higher risk for
the illness than those born before 1960.
Evidence
suggests an important role of sociocultural in-fluences in the development of
bulimia nervosa. For example, the frequency of the disorder has been reported
to be increasing among immigrants to the USA and UK from nonWestern coun-tries
(Hsu, 1990). Although the rate of the disorder appears to be lower among
nonwhite and nonWestern cultures, the frequency of bulimia nervosa has been
reported to be increasing among these groups, especially among the higher
socioeconomic classes. Sur-prisingly, several epidemiological and clinical
studies in the USA found no relationship between bulimia nervosa and social
class (Kendler et al., 1991).
Among
patients with bulimia nervosa who are seen at eat-ing disorders clinics, there
is an increased frequency of anxiety and mood disorders, especially major
depressive disorder and dysthymic disorder, of drug and alcohol abuse, and of
personal-ity disorders. It is not certain whether this comorbidity is also
observed in community samples or whether it is a characteristic of individuals
who seek treatment.
Etiology
As in the
case of anorexia nervosa, the etiology of bulimia ner-vosa is uncertain.
Several factors clearly predispose individuals to the development of bulimia
nervosa, including being an ado-lescent girl or young adult woman. A personal
or family history of obesity and of mood disturbance also appears to increase
risk. Twin studies have suggested that inherited factors are related to the
risk of developing bulimia nervosa, but what these factors are and how they
operate are unclear.
Many of
the same psychosocial factors related to the de-velopment of anorexia nervosa
are also applicable to bulimia ner-vosa, including the influence of cultural
esthetic ideals of thinness and physical fitness. Similarly, bulimia nervosa
primarily affects women; the ratio of men to women is approximately 1 : 10. It
also
occurs
more frequently in certain occupations (e.g., modeling) and sports (e.g.,
wrestling, running).
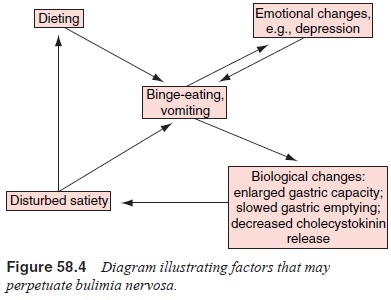
Although
not proven, it seems likely that several fac-tors serve to perpetuate the
binge-eating once it has begun (Figure 58.4 First, most individuals with
bulimia nervosa, be-cause of both their concern regarding weight and their
worry about the effect of the binge-eating, attempt to restrict their food
intake when they are not binge-eating. The psychological and physiological restraint
that is thereby entailed presumably makes additional binge-eating more likely.
Secondly, even if mood disturbance is not present at the outset, individuals
be-come distressed about their inability to control their eating, and the
resultant lowering of self-esteem contributes to dis-turbances of mood and to a
reduced ability to control impulses to overeat. In addition,
cognitive–behavioral theories empha-size the role of rigid rules regarding food
and eating, and the distorted and dysfunctional thoughts that are similar to
those seen in anorexia nervosa. Interpersonal theories also impli-cate
interpersonal stressors as a primary factor in triggering binge-eating. There
is no evidence to suggest that a particular personality structure is
characteristic of women with bulimia nervosa.
There are
also indications that bulimia nervosa is accom-panied by physiological
disturbances that disrupt the develop-ment of satiety during a meal and
therefore increase the likeli-hood of binge-eating. These disturbances include
an enlarged stomach capacity, a delay in stomach emptying and a reduction in
the release of cholecystokinin, a peptide hormone secreted by the small
intestine during a meal that normally plays a role in terminating eating
behavior. All these abnormalities appear to predispose the individual to
overeat and therefore to perpetuate the cycle of binge-eating.
It has been suggested that childhood sexual abuse is a specific risk factor for the development of bulimia nervosa. Sci-entific support for this hypothesis is weak. The best studies to date have found that compared with women without psychiatric illness, women with bulimia nervosa do indeed report increased frequencies of sexual abuse. However, the rates of abuse are similar to those found in other psychiatric disorders and occur in a minority of women with bulimia nervosa. Thus, while early abuse may predispose an individual to psychiatric problems gen-erally, it does not appear to lead specifically to an eating disorder and most patients with bulimia nervosa do not have histories of sexual abuse
Pathophysiology
In a
small fraction of individuals, bulimia nervosa is associated with the
development of fluid and electrolyte abnormalities that result from the
self-induced vomiting or the misuse of laxatives or diuretics. The most common
electrolyte disturbances are hy-pokalemia, hyponatremia and hypochloremia.
Patients who lose substantial amounts of stomach acid through vomiting may
be-come slightly alkalotic; those who abuse laxatives may become slightly
acidotic.
There is
an increased frequency of menstrual disturbances such as oligomenorrhea among
women with bulimia nervosa. Sev-eral studies suggest that the
hypothalamic–pituitary–gonadal axis is subject to the same type of disruption
as is seen in anorexia ner-vosa but that the abnormalities are much less
frequent and severe.
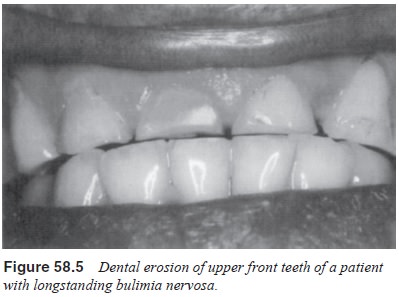
Patients
who induce vomiting for many years may develop dental erosion, especially of
the upper front teeth (Figure 58.5). The mechanism appears to be that stomach
acid softens the enamel, which in time gradually disappears so that the teeth
chip more easily and can become reduced in size. Some patients de-velop
painless salivary gland enlargement, which is thought to represent hypertrophy
resulting from the repeated episodes of binge-eating and vomiting. The serum
level of amylase is some-times mildly elevated in patients with bulimia nervosa
because of increased amounts of salivary amylase.
Most
patients with bulimia nervosa have surprisingly few gastrointestinal
abnormalities. As indicated earlier, it appears that the disorder is associated
with an enlarged gastric capacity and delayed gastric emptying, but these
abnormalities are not so severe as to be detectable on routine clinical
examination. Poten-tially life-threatening complications such as an esophageal
tear or gastric rupture occur, but fortunately rarely.
The
longstanding use of syrup of ipecac to induce vomit-ing can lead to absorption
of some of the alkaloids and to perma-nent damage to nerve and muscle.
Related Topics