Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Basal Cell and Squamous Cell Carcinoma
BASAL CELL AND SQUAMOUS CELL CARCINOMA
The most common types of skin cancer are basal cell
carcinoma (BCC) and squamous cell (epidermoid) carcinoma (SCC). The third most
common type, malignant melanoma, is discussed sepa-rately. Skin cancer is
diagnosed by biopsy and histologic evaluation.
Clinical Manifestations
BCC
is the most common type of skin cancer. It generally ap-pears on sun-exposed
areas of the body and is more prevalent in regions where the population is
subjected to intense and exten-sive exposure to the sun. The incidence is
proportional to the age of the patient (average age of 60 years) and the total
amount of sun exposure, and it is inversely proportional to the amount of
melanin in the skin.
BCC usually begins as a small, waxy nodule with rolled, trans-lucent, pearly borders; telangiectatic vessels may be present. As it grows, it undergoes central ulceration and sometimes crusting (Fig. 56-6). The tumors appear most frequently on the face. BCC is characterized by invasion and erosion of contiguous (adjoin-ing) tissues. It rarely metastasizes, but recurrence is common. However, a neglected lesion can result in the loss of a nose, an ear, or a lip. Other variants of BCC may appear as shiny, flat, gray or yellowish plaques.
SCC
is a malignant proliferation arising from the epidermis. Although it usually
appears on sun-damaged skin, it may arise from normal skin or from preexisting
skin lesions. It is of greater concern than BCC because it is a truly invasive
carcinoma, metas-tasizing by the blood or lymphatic system.
Metastases
account for 75% of deaths from SCC. The lesions may be primary, arising on the
skin and mucous membranes, or they may develop from a precancerous condition,
such as actinic keratosis (ie, lesions occurring in sun-exposed areas),
leukoplakia (ie, premalignant lesion of the mucous membrane), or scarred or
ulcerated lesions. SCC appears as a rough, thickened, scaly tumor that may be
asymptomatic or may involve bleeding (see Fig. 56-6). The border of an SCC
lesion may be wider, more infiltrated, and more inflammatory than that of a BCC
lesion. Secondary infec-tion can occur. Exposed areas, especially of the upper
extremities and of the face, lower lip, ears, nose, and forehead, are common
sites (Odom et al., 2000).
Prognosis
The
prognosis for BCC is usually good. Tumors remain localized, and although some
require wide excision with resultant dis-figurement, the risk for death from
BCC is low. The prognosis for SCC depends on the incidence of metastases, which
is related to the histologic type and the level or depth of invasion. Usually,
tu-mors arising in sun-damaged areas are less invasive and rarely cause death,
whereas SCC that arises without a history of sun or arsenic exposure or scar
formation appears to have a greater chance for spread. Regional lymph nodes
should be evaluated for metas-tases (Odom et al., 2000).
Medical Management
The
goal of treatment is to eradicate the tumor. The treatment method depends on
the tumor location; the cell type, location, and depth; the cosmetic desires of
the patient; the history of pre-vious treatment; whether the tumor is invasive,
and whether metastatic nodes are present. The management of BCC and SCC
includes surgical excision, MohsŌĆÖ micrographic surgery, electro-surgery,
cryosurgery, and radiation therapy.
SURGICAL MANAGEMENT
The
primary goal is to remove the tumor entirely. The best way to maintain cosmetic
appearance is to place the incision properly along natural skin tension lines
and natural anatomic body lines. In this way, scars are less noticeable. The
size of the incision de-pends on the tumor size and location but usually
involves a length-to-width ratio of 3 1.
The
adequacy of the surgical excision is verified by micro-scopic evaluation of
sections of the specimen. When the tumor is large, reconstructive surgery with
use of a skin flap or skin graft-ing may be required. The incision is closed in
layers to enhance cosmetic effect. A pressure dressing applied over the wound
pro-vides support. Infection after a simple excision is uncommon if proper
surgical asepsis is maintained.
MohsŌĆÖ Micrographic Surgery.
MohsŌĆÖ micrographic surgery is thetechnique that is most accurate and that
best conserves normal tissue. When the surgical technique was introduced, the
excision followed an application of zinc chloride paste to the tumor, but MohsŌĆÖ
surgery is now performed without the initial chemo-surgery component. The
procedure removes the tumor layer by layer. The first layer excised includes
all evident tumor and a small margin of normal-appearing tissue. The specimen
is frozen and analyzed by section to determine if all the tumor has been
re-moved. If not, additional layers of tissue are shaved and examined until all
tissue margins are tumor free. In this manner, only the tumor and a safe,
normal-tissue margin are removed. MohsŌĆÖ surgery is the recommended
tissue-sparing procedure, with cure rates for BCC and SCC approaching 99%. It
is the treatment of choice and the most effective for tumors around the eyes,
nose, upper lip, and auricular and periauricular areas (Odom et al., 2000).
Electrosurgery.
Electrosurgery is the destruction or removal of
tissue by electrical energy. The current is converted to heat, which then
passes to the tissue from a cold electrode. Electrosurgery may be preceded by
curettage (ie, excising the skin tumor by scraping its surface with a curette).
Electrodesiccation is then implemented to achieve hemostasis and to destroy any
viable malignant cells at the base of the wound or along its edges.
Electrodesiccation is use-ful for lesions smaller than 1 to 2 cm (0.4 to 0.8
in) in diameter.
This
method takes advantage of the fact that the tumor in each instance is softer
than surrounding skin and therefore can be out-lined by a curette, which
ŌĆ£feelsŌĆØ the extent of the tumor. The tumor is removed and the base cauterized.
The process is repeated twice. Usually, healing occurs within a month.
Cryosurgery.
Cryosurgery destroys the tumor by deep freezingthe tissue. A thermocouple
needle apparatus is inserted into the skin, and liquid nitrogen is directed to
the center of the tumor until the tumor base is ŌłÆ40┬░C to ŌłÆ60┬░C. Liquid
nitrogen has the lowest boiling point of all cryogens tried, is inexpensive,
and is easy to obtain. The tumor tissue is frozen, allowed to thaw, and then
refrozen. The site thaws naturally and then becomes gelati-nous and heals spontaneously.
Swelling and edema follow the freezing. The appearance of the lesion varies.
Normal healing, which may take 4 to 6 weeks, occurs faster in areas with a good
blood supply.
RADIATION THERAPY
Radiation
therapy is frequently performed for cancer of the eye-lid, the tip of the nose,
and areas in or near vital structures (eg, fa-cial nerve). It is reserved for
older patients, because x-ray changes may be seen after 5 to 10 years, and
malignant changes in scars may be induced by irradiation 15 to 30 years later.
The
patient should be informed that the skin may become red and blistered. A bland
skin ointment prescribed by the physician may be applied to relieve discomfort.
The patient should also be cautioned to avoid exposure to the sun.
Nursing Management
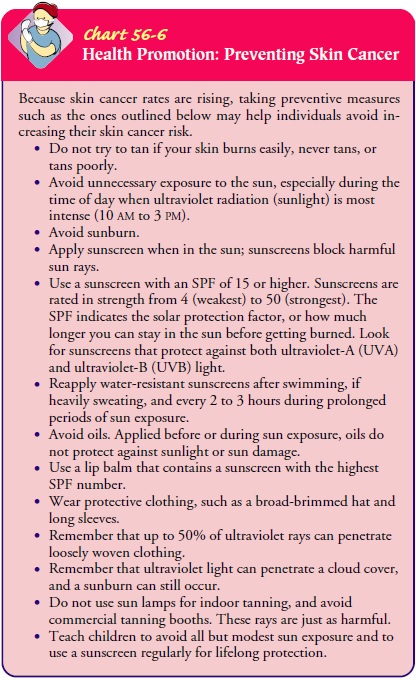
Because
many skin cancers are removed by excision, patients are usually treated in
outpatient surgical units. The role of the nurse is to teach the patient about
prevention of skin cancer and about self-care after treatment (Chart 56-6).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
The wound is usually covered with a dressing to
protect the site from physical trauma, external irri-tants, and contaminants.
The patient is advised when to report for a dressing change or is given written
and verbal information on how to change dressings, including the type of
dressing to pur-chase, how to remove dressings and apply fresh ones, and the
im-portance of hand washing before and after the procedure.
The
patient is advised to watch for excessive bleeding and tight dressings that
compromise circulation. If the lesion is in the peri-oral area, the patient is
instructed to drink liquids through a straw and limit talking and facial
movement. Dental work should be avoided until the area is completely healed.
After the sutures are removed, an emollient cream may be used to help reduce dryness. Applying a sunscreen over the wound is advised to prevent postoperative hyperpigmentation if the patient spends time outdoors.
Follow-up examinations should be at regular
intervals, usually every 3 months for a year, and should include palpation of
the ad-jacent lymph nodes. The patient should also be instructed to seek
treatment for any moles that are subject to repeated friction and irritation,
and to watch for indications of potential malignancy in moles as described
previously. The importance of lifelong fol-low-up evaluations should be
emphasized.
Teaching About Prevention.
Studies show that regular daily useof a sunscreen with a solar protection
factor (SPF) of at least 15 can reduce the recurrence of skin cancer by as much
as 40%. The sunscreen should be applied to head, neck, arms, and hands every
morning at least 30 minutes before leaving the house and reap-plied every 4
hours if the skin perspires. Discretionary application (ie, applied only when
sun exposure is anticipated) has not shown the same preventive response
(Barton, 2001).
Related Topics