Chapter: Medical Surgical Nursing: Assessment and Management of Problems Related to Male Reproductive Processes
Assessment of Problems Related to Male Reproductive Processes
Assessment
HEALTH HISTORY AND CLINICAL MANIFESTATIONS
Assessment
of male reproductive function begins with an evalu-ation of urinary function
and symptoms. This assessment also in-cludes a focus on sexual function as well
as manifestations of sexual dysfunction. The patient is asked about his usual
state of health and any recent change in general physical and sexual ac-tivity.
Any symptoms or changes in function are explored fully and described in detail.
These symptoms may include those as-sociated with an obstruction caused by an
enlarged prostate gland: increased urinary frequency, decreased force of urine
stream, “double” or “triple” voiding (the patient needs to urinate two or three
times over a period of several minutes to completely empty his bladder). The
patient is also assessed for dysuria, hema-turia, and hematospermia (blood in
the ejaculate).
Assessment
of sexual function and dysfunction is an essential part of every health
history. The extent of the history will depend on the patient’s presenting
symptoms and the presence of factors that may affect sexual function: chronic
illnesses (eg, diabetes,multiple sclerosis, stroke, cardiac disease), use of
medications that affect sexual function (eg, many antihypertensive and
anti-cholesterolemic medications, psychotropic agents), stress, and alcohol
use.
Discussing
sexuality with patients with an illness or disability can be uncomfortable for
nurses and other health care providers. Health care professionals may
unconsciously have stereotypes re-lated to sexuality about people who are ill
or disabled (eg, ill or disabled persons are asexual or should remain sexually
inactive). In addition, patients are often embarrassed to initiate a discussion
about these issues with their health care providers (Hughes, 2000). Because
changes in sexual functioning are a common con-cern of patients, it is
important to address these issues when ob-taining the health history. By
initiating an assessment about sexual concerns, the nurse demonstrates that
changes in sexual functioning are valid topics for discussion and provides a
safe environment for discussing these sensitive topics. The PLISSIT
(permission, limited information, specific suggestions, intensive therapy)
model of sexual assessment and intervention may be used to provide a framework
for nursing interventions (Annon, 1976). This model begins by asking the
patient’s permission to discuss sexual functioning. Limited information about
sexual function may then be provided to the patient. As the discussion
progresses, the nurse may offer specific suggestions for interven-tions. For
some individuals, a professional who specializes in sex therapy may provide
more intensive therapy as needed.
PHYSICAL ASSESSMENT
In
addition to the customary aspects of the physical examination, two essential
components address disorders of the male genital or reproductive system: the
digital rectal examination and the tes-ticular examination.
Digital Rectal Examination
The
digital rectal examination (DRE) is recommended as part of the regular health
checkup for every man older than 40 years of age; it is invaluable in screening
for cancer of the prostate gland. The DRE enables the examiner to assess the
size, shape, and consistency of the prostate gland (Fig. 49-2). Tenderness of
the prostate gland on palpation and the presence and consis tency of any
nodules are noted. Although having this examina-tion may be embarrassing for
the patient, it is an important screening tool.
Testicular Examination
The
male genitalia are inspected for abnormalities and palpated for masses. The
scrotum is palpated carefully for nodules, masses, or inflammation. Examining
the scrotum can reveal such dis-orders as hydrocele, hernia, or tumor of the
testis. The penis is inspected and palpated for ulcerations, nodules,
inflammation, and discharge. The testicular examination provides an excellent
opportunity to instruct the patient about techniques for testic-ular
self-examination and its importance in early detection of testicular cancer.
This self-examination should begin during adolescence.
Gerontologic Considerations
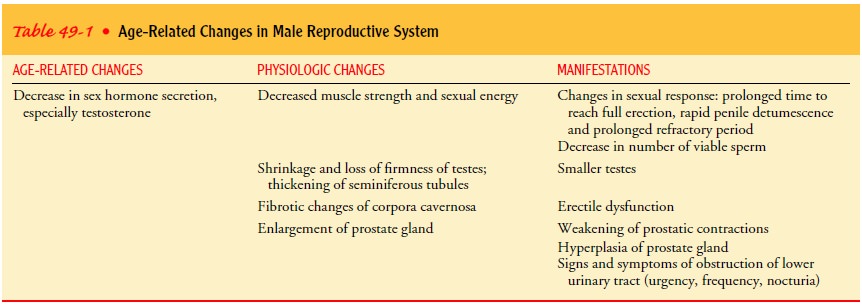
As men
age, the prostate gland enlarges, prostate secretion de-creases, the scrotum
hangs lower, the testes become smaller and more firm, and pubic hair becomes
sparser and stiffer. Changes in gonadal function include a decline in plasma
testosterone levels and reduced production of progesterone (Table 49-1). Other
changes include decreasing sexual function, slower sexual responses, an
increased incidence of genitourinary tract cancer, and urinary incontinence for
various reasons.
Male
reproductive capability is maintained with advancing age. Although degenerative
changes occur in the seminiferous tubules, spermatogenesis (production of
sperm) continues. Sexual function, however, involving libido (desire) and
potency, de-creases. Vascular problems cause about half of the cases of
impo-tence in men older than 50 years of age.
Hypogonadism occurs in up to one fourth of older men. The relationship of hypogonadism to impotence is uncertain. This de-cline is more evident in men older than 70 years but is also noted in men in their 60s. In older men, the sexual response slows. Erec-tion takes longer in men older than 50 years of age, and full erec-tions may not be attained until orgasm. Sexual function is affected by several factors, such as psychological problems, illnesses, and medications. In general, the sexual act takes longer. In older men, ejaculatory control increases; however, if the erection is partially lost, there may be difficulty in attaining a full erection again, and resolution may occur without orgasm.
Sexual activity is closely correlated with the man’s
sexual activity of his earlier years; if he was more active than average as a
young man, he will most likely continue to be more active than average in his
later years.
Cancers
of the kidney, bladder, prostate, and penis all have in-creased incidence in
men older than 50 years of age. DRE and screening tests for hematuria may
uncover a higher percentage of malignancies at earlier stages.
Urinary
incontinence in the elderly man may have many causes, including medications and
age-related conditions, such as neurologic diseases or benign prostatic hyperplasia (BPH; also referred to as hypertrophy
and called an enlarged prostate by the lay public). Diagnostic tests are
performed to exclude reversible causes of urinary incontinence. For some
patients with severe in-continence, augmentation cystoplasty (repair of the
bladder) with placement of an artificial urinary sphincter may help alleviate
this problem.
Related Topics