Chapter: Medical Surgical Nursing: Assessment and Management of Female Physiologic Processes
Assessment of Female Physiologic Processes: Physical Assessment
PHYSICAL
ASSESSMENT
Periodic
examinations and routine cancer screening are important for all women. An
annual breast and pelvic examination is im-portant for all women age 18 or
older and for those who are sex-ually active, regardless of age. The patient
deserves understanding and support because of the emotional and physical
considerations associated with gynecologic examinations. Women may be sensi-tive
or embarrassed by the usual questions asked by a gynecologist or women’s health
care provider. Because gynecologic conditions are of a personal and private
nature to most women, such infor-mation is shared only with those directly
involved in patient care (as is true with all patient information).
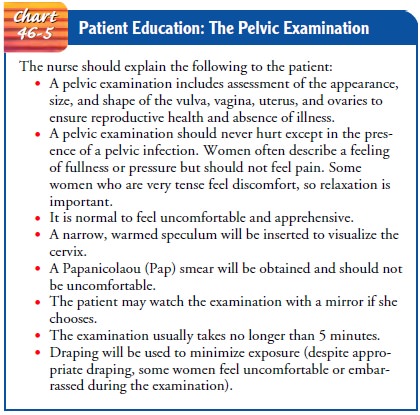
Throughout
the examination, the nurse explains the proce-dures to be performed. This not
only encourages the woman to relax but also provides an opportunity for her to
ask questions and minimizes the negative feelings that many women associate
with gynecologic examinations.
The
first pelvic examination is often anxiety-producing for women; the nurse can
alleviate many of these feelings with expla-nations and teaching (Chart 46-5).
Before the examination begins, the patient is asked to empty her bladder and to
provide a urine specimen if urine tests are part of the total assessment.
Voiding en-sures patient comfort and eases the examination because a full
bladder can make palpation of pelvic organs uncomfortable for the patient and
difficult for the examiner.
Positioning
Although
several positions may be used for the pelvic examination, the supine lithotomy
position is used most commonly, although the upright lithotomy position (in
which the woman assumes a semisitting posture) may also be used. This position
offers several advantages:
· It is more comfortable
for some women.
· It allows better eye
contact between patient and examiner.
· It may provide an easier
means for the examiner to carry out the bimanual examination.
· It enables the woman to use a mirror to see her anatomy (if she chooses) to visualize any conditions that require treatment or to learn about using certain types of contraceptive methods.
In the
supine lithotomy position, the patient lies on the table with her feet on foot
rests or stirrups. She is encouraged to relax so that her buttocks are
positioned at the edge of the examination table, and she is asked to relax and
spread her thighs as widely apart as possible.
If the patient is too ill, disabled, or neurologically impaired to lie safely on the examination table or cannot maintain the supine litho-tomy position, the Sims’ position may be used. In Sims’ position, the patient lies on her left side with her right leg bent at a 90-degree angle. The right labia may be retracted to gain adequate access to the vagina. Other positions for pelvic examination for disabled women make the examination easier for the woman and the clini-cian. The presence of a disability does not justify skipping any parts of the physical assessment, including the pelvic examination.
The
following equipment is obtained and readily available: a good light source; a
vaginal speculum; clean examination gloves; lubricant, spatula, cytobrush,
glass slides, fixative solution or spray; and diagnostic testing supplies for
screening for occult rectal blood if the woman is older than 40. Latex-free
gloves should be avail-able if the patient or clinician is allergic to latex.
This allergy is be-coming more prevalent in nurses and other health care
providers and patients and is potentially life-threatening. Patients should be
questioned about previous reactions to latex.
Inspection
After
the patient is prepared, the examiner inspects the labia ma-jora and minora,
noting the epidermal tissue of the labia majora; the skin fades to the pink
mucous membrane of the vaginal in-troitus. Lesions of any type (eg, venereal
warts, pigmented lesions [melanoma]) are evaluated. In the nulliparous woman,
the labia minora come together at the opening of the vagina. In women who have
delivered children vaginally, the labia minora may gape and vaginal tissue may
protrude.
Trauma
to the anterior vaginal wall during childbirth may have resulted in
incompetency of the musculature, and a bulge caused by the bladder protruding
into the submucosa of the an-terior vaginal wall (cystocele) may be seen. Childbirth trauma may also have affected
the posterior vaginal wall, producing a bulge caused by rectal cavity
protrusion (rectocele). The cervix
may descend under pressure through the vaginal canal and be seen at the
introitus (uterine prolapse). To
identify such protrusions, the examiner asks the patient to “bear down.”
The
introitus should be free of superficial mucosal lesions. The labia minora may
be separated by the fingers of the gloved hand and the lower part of the vagina
palpated. In virgins, a hymen of
variable thickness may be felt circumferentially within 1 or 2 cm of the
vaginal opening. The hymenal ring usually permits the insertion of one finger.
Rarely, the hymen totally occludes the vaginal entrance (imperforate hymen).
In
women who are not virgins, a rim of scar tissue represent-ing the remnants of
the hymenal ring may be felt circumferen-tially around the vagina near its
opening. The greater vestibular glands (Bartholin’s glands) lie between the
labia minora and the remnants of the hymenal ring. An abscess of the
Bartholin’s gland can cause discomfort and requires incision and drainage.
Speculum Examination
The
bivalved speculum, either metal or plastic, is available in many sizes. Metal
specula are soaked, scrubbed, and sterilized be-tween patients. Some clinicians
and some patients prefer plastic specula, which permit one-time use. The
speculum should be warmed with a heating pad or warm water to make insertion
more comfortable for the patient. The speculum is not lubricated because
commercial lubricants interfere with cervical cytology (Papanicolaou [Pap]
smear) findings.
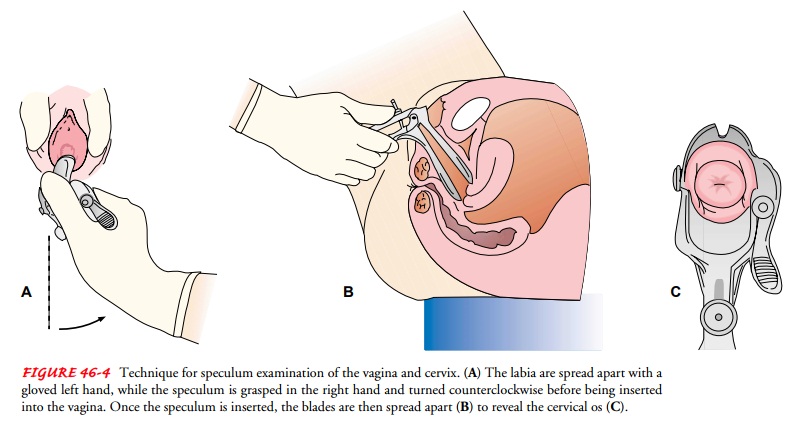
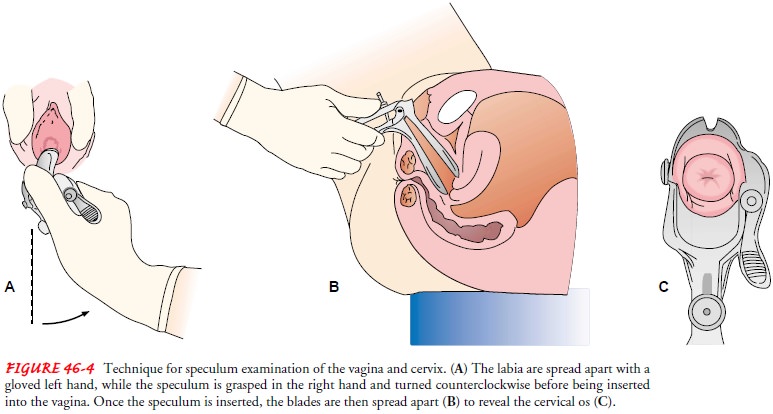
The metal
speculum has two set-screws. The one along the handle, holding the two valves
of the speculum together, is kept tightened. The screw that holds the thumb
rest in place is loos-ened. The speculum is grasped in the dominant hand, with
the thumb against the back of the thumb rest to keep the tips of the valves
closed. The speculum is rotated slightly counterclockwise, and the vaginal
orifice is held open by the thumb and the fore-finger of the gloved nondominant
hand by some examiners. Other examiners find that straight insertion of a
speculum with downward pressure on the vagina is more comfortable for the
pa-tient. The speculum is gently inserted into the posterior portion of the
introitus and slowly advanced to the top of the vagina; this should not be
painful or uncomfortable for the woman. The tip of the speculum may then be
elevated and the speculum rotated to a transverse position. The speculum is
then slowly opened and the set-screw of the thumb rest is tightened to hold the
speculum open (Fig. 46-4).
CERVIX
The
cervix is inspected. In nulliparous women, the cervix usually is 2 to 3 cm wide
and smooth. Women who have borne children may have a laceration, usually
transverse, giving the cervical os a “fishmouth” appearance. Epithelium from
the endocervical canal may have grown onto the surface of the cervix, appearing
as beefy-red surface epithelium circumferentially around the os. Occasion-ally,
the cervix of a woman whose mother took DES has a hooded appearance (a peaked
aspect superiorly or a ridge of tissue sur-rounding it); this is evaluated by
colposcopy when identified.
ABNORMAL GROWTH
Malignant changes may not be obviously
differentiated from the rest of the cervical mucosa. Small, benign cysts may
appear on the cervical surface. These are usually bluish or white and are
called nabothian cysts. A polyp of
endocervical mucosa may protrude through the os and usually is dark red. Polyps
can cause irregular bleeding; they are rarely malignant and usually are removed
eas-ily in an office or clinic setting. A carcinoma may appear as a
cauliflower-like growth that bleeds easily when touched. Bluish col-oration of
the cervix is a sign of early pregnancy (Chadwick’s sign).
PAP SMEAR
During the pelvic examination, a Pap smear is
obtained by rotat-ing a small spatula at the os, followed by a cervical brush
rotated in the os. The tissue obtained is spread on a glass slide and sprayed
or fixed immediately, or inserted into a liquid. A small broom-like device can
also be used to obtain specimens for the Pap smear.
A specimen of any purulent material appearing at the cervical os is obtained for culture. A sterile applicator is used to obtain the specimen, which is immediately placed in an appropriate medium for transfer to a laboratory. In patients at high risk for infection, routine cultures for gonococcal and chlamydial organisms are rec-ommended because of the high incidence of both diseases and the high risk for pelvic infection, fallopian tube damage, and sub-sequent infertility.
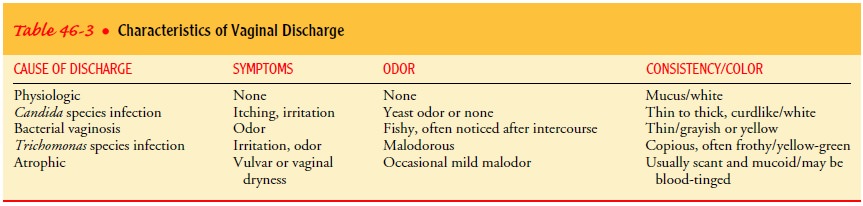
Vaginal
discharge, which may be normal or may result from vaginitis, may be present.
Discharge caused by bacteria (bacterial vaginosis) usually appears gray and
purulent. Discharge caused by Trichomonas
species infection is usually frothy, copious, and mal-odorous. Discharge
caused by Candida species infection
is usu-ally thick and white-yellow and has a cottage-cheese appearance. Table
46-3 summarizes the characteristics of vaginal discharge found in different
conditions.
The
vagina is inspected as the examiner withdraws the specu-lum. It is smooth in
young girls and thickens after puberty, with many rugae (folds) and redundancy
in the epithelium. In meno-pausal women, the vagina thins and has fewer rugae
because of decreased estrogen.
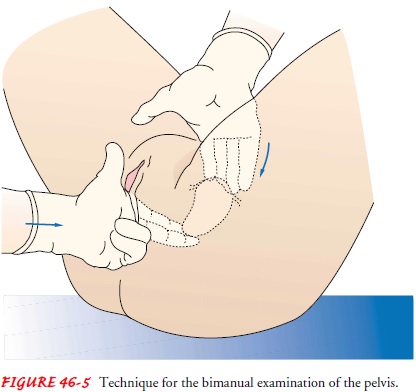
Bimanual Palpation
To
complete the pelvic examination, the examiner performs a bi-manual examination
from a standing position. The examination is performed with the forefinger and
middle finger of the gloved and lubricated hand. These fingers are placed in
the vaginal ori-fice, while the other fingers are held tightly out of the way,
with the thumb completely adducted. The fingers are advanced verti-cally along
the vaginal canal, and the vaginal wall is palpated. Any firm part of the
vaginal wall may represent old scar tissue from childbirth trauma but may also
require further evaluation.
CERVICAL PALPATION
The
cervix is palpated and assessed for its consistency, mobility, size, and
position. The normal cervix is uniformly firm but not hard. Softening of the
cervix is a finding in early pregnancy. Hardness and immobility of the cervix
may reflect invasion by a neoplasm. Pain on gentle movement of the cervix is
called a pos-itive chandelier sign
or positive cervical motion tenderness (recorded as +CMT)
and usually indicates a pelvic infection.
UTERINE PALPATION
To
palpate the uterus, the examiner places the opposite hand on the abdominal wall
halfway between the umbilicus and the pubis and presses firmly toward the
vagina (Fig. 46-5). Movement of the abdominal wall causes the body of the
uterus to descend, and the pear-shaped organ becomes freely movable between the
ab-dominal examining hand and the fingers of the pelvic examining hand. Uterine
size, mobility, and contour can be estimated through palpation. Fixation of the
uterus in the pelvis may be a sign of endometriosis
or malignancy.
The body of the uterus is normally twice the diameter and twice the length of the cervix, curving anteriorly toward the abdominal wall. Some women have a retroverted or retroflexed uterus, which tips posteriorly toward the sacrum, whereas others have a uterus that is neither anterior nor posterior but is midline.
ADNEXAL PALPATION
Next,
the right and left adnexal areas are palpated to evaluate the fallopian tubes
and ovaries. The fingers of the hand examining the pelvis are moved first to
one side, then to the other, while the hand palpating the abdominal area is
moved correspondingly to either side of the abdomen and downward. The adnexa
(ovaries and fallopian tubes) are trapped between the two hands and pal-pated
for an obvious mass, tenderness, and mobility. Commonly, the ovaries are
slightly tender, and the patient is informed that slight discomfort on
palpation is normal.
VAGINAL AND RECTAL PALPATION
Bimanual palpation of the vagina and cul-de-sac is accomplished by placing the index finger in the vagina and the middle finger in the rectum. To prevent cross-contamination between the vaginal and rectal orifices, the examiner puts on new gloves. A gentle movement of these fingers toward each other compresses the pos-terior vaginal wall and the anterior rectal wall and assists the ex-aminer in identifying the integrity of these structures. During this procedure, the patient may sense an urge to defecate. The nurse assures the patient that this is unlikely to occur. Ongoing expla-nations are provided to reassure and educate the patient about the procedure.
Gerontologic Considerations
Yearly
examinations can help prevent problems of the repro-ductive tract in aging
women. Some older women do not have regular gynecologic examinations. If a
woman delivered her chil-dren at home, she may never have had a pelvic
examination. Some regard it as an embarrassing and unpleasant procedure. An
im-portant role of the nurse is to encourage an annual gynecologic examination
for all women. The nurse can make the examina-tion a time for education and
reassurance rather than a time of embarrassment.
Perineal
pruritus is common in elderly women and should be evaluated because it may
indicate a disease process (diabetes or malignancy). It may also indicate
vulvar dystrophy, a thickened or whitish discoloration of tissue that needs
biopsy to rule out ab-normal cells. Topical cortisone and hormone creams may be
pre-scribed for symptomatic relief.
With
relaxing pelvic musculature, uterine prolapse and re-laxation of the vaginal
walls can occur. Appropriate evaluation and surgical repair can provide relief
if the patient is a candidate for surgery. After surgery, the patient needs to
know that tissue repair and healing may require additional time. Pessaries
(latex devices that provide support) are often used if surgery is
con-traindicated or before surgery to see if surgery can be avoided. They are
fitted by a health care provider and may reduce dis-comfort and pressure. Use
of a pessary requires the patient to have routine gynecologic examinations to
monitor for irritation or infection.
Related Topics