Chapter: Medical Surgical Nursing: Management of Patients With Chest and Lower Respiratory Tract Disorders
Aspiration
Aspiration
Aspiration
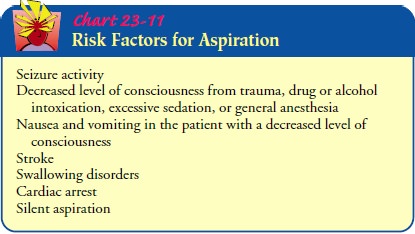
of stomach contents into the lungs is a serious com-plication that may cause
pneumonia and result in the following clinical picture: tachycardia, dyspnea,
central cyanosis, hyperten-sion, hypotension, and finally death. It can occur
when the pro-tective airway reflexes are decreased or absent from a variety of
factors (Chart 23-11).
Pathophysiology
The
primary factors responsible for death and complications after aspiration of
gastric contents are the volume and character of the aspirated gastric
contents. For example, a small, localized aspira-tion from regurgitation can
cause pneumonia and acute respira-tory distress; a massive aspiration is
usually fatal.
A full stomach contains solid particles of food. If these are as-pirated, the problem then becomes one of mechanical blockage of the airways and secondary infection. During periods of fasting, the stomach contains acidic gastric juice, which, if aspirated, may be very destructive to the alveoli and capillaries. Fecal contami-nation (more likely seen in intestinal obstruction) increases the likelihood of death because the endotoxins produced by intesti-nal organisms may be absorbed systemically, or the thick pro-teinaceous material found in the intestinal contents may obstruct the airway, leading to atelectasis and secondary bacterial invasion.
Aspiration
pneumonitis may develop from aspiration of sub-stances with a pH of less than
2.5 and a volume of gastric aspirate greater than 0.3 mL per kilogram of body
weight (20 to 25 mL in adults) (Marik, 2001). Aspiration of gastric contents causes
a chemical burn of the tracheobronchial tree and pulmonary parenchyma (Marik,
2001). An inflammatory response occurs. This results in the destruction of
alveolar–capillary endothelial cells, with a consequent outpouring of
protein-rich fluids into the interstitial and intra-alveolar spaces. As a
result, surfactant is lost, which in turn causes the airways to close and the
alveoli to col-lapse. Finally, the impaired exchange of oxygen and carbon
diox-ide causes respiratory failure.
Aspiration
pneumonia develops following inhalation of colo-nized oropharyngeal material.
The pathologic process involves an acute inflammatory response to bacteria and
bacterial products. Most commonly, the bacteriologic findings include
gram-positive cocci, gram-negative rods, and occasionally anaerobic bacteria
(Marik, 2001).
Prevention
Prevention
is the primary goal when caring for patients at risk for aspiration.
COMPENSATING FOR ABSENT REFLEXES
Aspiration
is likely to occur if the patient cannot adequately co-ordinate protective
glottic, laryngeal, and cough reflexes. This hazard is increased if the patient
has a distended abdomen, is in a supine position, has the upper extremities
immobilized by in-travenous infusions or hand restraints, receives local
anesthetics to the oropharyngeal or laryngeal area for diagnostic procedures,
has been sedated, or has had long-term intubation.
When
vomiting, a person can normally protect the airway by sitting up or turning on
the side and coordinating breathing, coughing, gag, and glottic reflexes. If
these reflexes are active, an oral airway should not be inserted. If an airway
is in place, it should be pulled out the moment the patient gags so as not to
stimulate the pharyngeal gag reflex and promote vomiting and as-piration.
Suctioning of oral secretions with a catheter should be performed with minimal
pharyngeal stimulation.
ASSESSING FEEDING TUBE PLACEMENT
Even when the patient is intubated, aspiration may occur even with a nasogastric tube in place. This aspiration may result in nosocomial pneumonia. Assessment of tube placement is key to prevent aspiration. The best method for determining tube place-ment is via an x-ray. There are other nonradiologic methods that have been studied. Observation of the aspirate and testing of its pH are the most reliable. Gastric fluid may be grassy green, brown, clear, or colorless. An aspirate from the lungs may be off-white or tan mucus. Pleural fluid is watery and usually straw-colored (Metheny & Titler, 2001). Gastric pH values are typically lower or more acidic that that of the intestinal or respiratory tract. Gastric pH is usually between 1 and 5, while intestinal or respi-ratory pH is 7 or higher (Metheny & Titler, 2001). There are dif-ferences in assessing tube placement with continuous versus intermittent feedings. For intermittent feedings with small-bore tubes, observation of aspirated contents and pH evaluation should be performed. For continuous feedings, the pH method is not clinically useful due to the infused formula (Metheny & Titler, 2001).
The
patient who is receiving continuous or timed-interval tube feedings must be
positioned properly. The patient receiving a con-tinuous infusion is given
small volumes under low pressure in an upright position, which helps to prevent
aspiration. Patients re-ceiving tube feedings at timed intervals are maintained
in an up-right position during the feeding and for a minimum of 30 minutes
afterward to allow the stomach to empty partially. Tube feedings must be given
only when it is certain that the feeding tube is posi-tioned correctly in the
stomach. Many patients today receive en-teral feeding directly into the
duodenum through a small-bore flexible feeding tube or surgically implanted
tube. Feedings are given slowly and regulated by a feeding pump. Correct
placement is confirmed by chest x-ray.
IDENTIFYING DELAYED STOMACH EMPTYING
A
full stomach may cause aspiration because of increased intra-gastric or
extragastric pressure. The following clinical situations cause a delayed
emptying time of the stomach and may con-tribute to aspiration: intestinal
obstruction; increased gastric secretions in gastroesophageal reflex disease;
increased gastric se-cretions during anxiety, stress, or pain; or abdominal distention
because of ileus, ascites, peritonitis, use of opioids and sedatives, severe
illness, or vaginal delivery.
When
a feeding tube is present, contents are aspirated, usually every 4 hours, to
determine the amount of the last feeding left in the stomach (residual volume).
If more than 50 mL is aspirated, there may be a problem with delayed emptying,
and the next feeding should be delayed or the continuous feeding stopped for a
period of time.
MANAGING EFFECTS OF PROLONGED INTUBATION
Prolonged
endotracheal intubation or tracheostomy can depress the laryngeal and glottic
reflexes because of disuse. Patients with prolonged tracheostomies are
encouraged to phonate and exer-cise their laryngeal muscles. For patients who
have had long-term intubation or tracheostomies, it may be helpful to have a
reha-bilitation therapist experienced in speech and swallowing disor-ders work
with the patient to assess the swallowing reflex.
Related Topics