Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Arteriosclerosis and Atherosclerosis
Management of Arterial Disorder
ARTERIOSCLEROSIS
AND ATHEROSCLEROSIS
Arteriosclerosis is the most common disease of the arteries; theterm means hardening of the arteries. It is a
diffuse process whereby the muscle fibers and the endothelial lining of the
walls of smallarteries
and arterioles become thickened. Atherosclerosis
involves a different process, affecting the intima of the large and medium-sized
arteries. These changes consist of the accumulation of lipids, calcium, blood
components, carbohydrates, and fibrous tissue on the intimal layer of the
artery. These accumulations are referred to as atheromas or plaques.
Although
the pathologic processes of arteriosclerosis and ath-erosclerosis differ,
rarely does one occur without the other, and the terms are often used
interchangeably. Because atherosclerosis is a generalized disease of the
arteries, when it is present in the ex-tremities, atherosclerosis is usually
present elsewhere in the body.
Pathophysiology
The
most common direct results of atherosclerosis in arteries in-clude narrowing
(stenosis) of the lumen, obstruction by throm-bosis, aneurysm, ulceration, and
rupture. Its indirect results are malnutrition and the subsequent fibrosis of
the organs that the sclerotic arteries supply with blood. All actively
functioning tis-sue cells require an abundant supply of nutrients and oxygen
and are sensitive to any reduction in the supply of these nutrients. If such
reductions are severe and permanent, the cells undergo is-chemic necrosis
(death of cells due to deficient blood flow) and are replaced by fibrous
tissue, which requires much less blood flow.
Atherosclerosis
can develop at any point in the body, but cer-tain sites are more vulnerable,
typically bifurcation or branch areas. In the proximal lower extremity, these
include the distal ab-dominal aorta, the common iliac arteries, the orifice of
the super-ficial femoral and profunda femoris arteries, and the superficial
femoral artery in the adductor canal. Distal to the knee, athero-sclerosis
occurs anywhere along the artery. There are no specific areas, such as arterial
bifurcations, that are more vulnerable for atherosclerosis.
Although
many theories exist about the development of ath-erosclerosis, no single theory
fully explains the pathogenesis; however, parts of several theories have been
combined into the reaction-to-injury theory. According to this theory, vascular
en-dothelial cell injury results from prolonged hemodynamic forces, such as
shearing stresses and turbulent flow, irradiation, chemi-cal exposure, or
chronic hyperlipidemia in the arterial system. In-jury to the endothelium
increases the aggregation of platelets and monocytes at the site of the injury.
Smooth muscle cells migrate and proliferate, allowing a matrix of collagen and
elastic fibers to form. It may be that there is no single cause or mechanism
for the development of atherosclerosis; rather, multiple processes may be
involved (Moore, 2002).
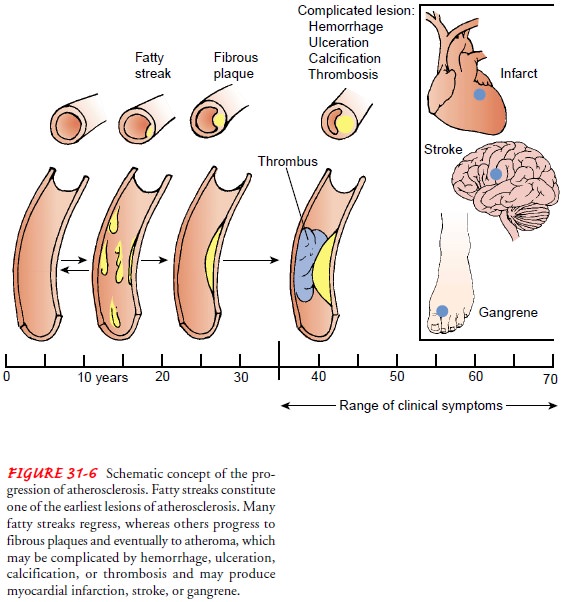
Morphologically,
atherosclerotic lesions are of two types: fatty streaks and fibrous plaque.
Fatty streaks are yellow and smooth, protrude slightly into the lumen of the
artery, and are composed of lipids and elongated smooth muscle cells. These
lesions have been found in the arteries of people of all age groups, including
infants. It is not clear whether fatty streaks predispose the person to the
formation of fibrous plaques or if they are reversible. They do not usually
cause clinical symptoms.
The
fibrous plaque characteristic of atherosclerosis is composed of smooth muscle
cells, collagen fibers, plasma components, and lipids. It is white to whitish
yellow and protrudes in various de-grees into the arterial lumen, sometimes completely
obstructing it. These plaques are found predominantly in the abdominal aorta
and the coronary, popliteal, and internal carotid arteries. This plaque is
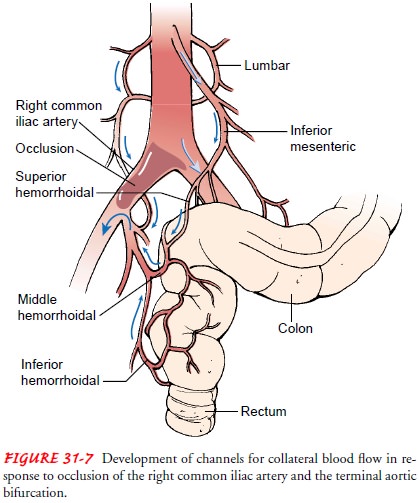
believed to be an irreversible lesion (Fig. 31-6). Gradual narrowing of the
arterial lumen as the disease process progresses stimulates the development of
collateral circulation
(Fig. 31-7). Collateral circulation consists of preexisting vessels that enlarge to reroute blood flow in the presence of a hemody-namically significant stenosis or occlusion. Collateral flow allows continued perfusion to the tissues beyond the arterial obstruction, but it is often inadequate to meet imposed metabolic demand, and ischemia results.
Risk Factors
Many
risk factors are associated with atherosclerosis (Chart 31-2). Although it is
not completely clear whether modification of these risk factors prevents the
development of cardiovascular disease, evidence indicates that it may slow the
disease process. Some risk factors, such as age or gender, cannot be modified.
However, it is believed that genetic factors can be modified indirectly by
alter-ing other risk factors (Moore, 2002).
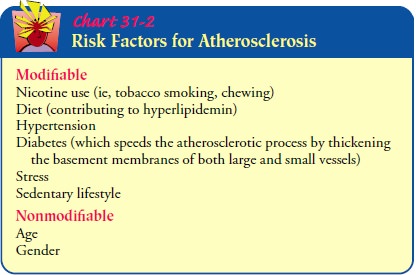
Tobacco use may be one of the strongest risk factors in the de-velopment of atherosclerotic lesions. Nicotine decreases blood flow to the extremities and increases heart rate and blood pressure by stimulating the sympathetic nervous system, causing vasocon-striction. It also increases the risk for clot formation by increasing the aggregation of platelets. Carbon monoxide, a toxin produced by burning tobacco, combines more readily with the hemoglobin than oxygen does, depriving the tissues of oxygen. The amount of tobacco use is directly related to the extent of the disease, and cessation of tobacco use reduces the risks. Many other factors such as obesity, stress, and lack of exercise have been identified as contributing to the disease process.
Prevention
Intermittent
claudication is a sign of generalized atherosclerosis and may be a marker of
occult coronary artery disease. Because a high-fat diet is suspected of
contributing to atherosclerosis, it is reasonable to measure serum cholesterol
and to begin prevention efforts. The American Heart Association recommends
reducing the amount of fat ingested in a healthy diet, substituting
unsatu-rated fats for saturated fats, and decreasing cholesterol intake to no
more than 300 mg daily to reduce the risk of cardiovascular disease (Krauss et
al., 2000).
Certain
medications combined with dietary modification and exercise are being used to
reduce blood lipid levels. There is limited evidence that these medications can
alter the course of peripheral arterial disease, but they may reduce the
mortality rate from cardio-vascular disease. Several classes of medication are
used to prevent atherosclerosis: bile acid sequestrants (cholestyramine
[Questran, Prevalite] or colestipol [Colestid]), nicotinic acid (niacin, B3, Nia-cor; Niaspan),
statins (atorvastatin [Lipitor], lovastatin [Mevacor], pravastatin [Pravachol],
simvastatin [Zocor]), fibric acids (gem-fibrozil [Lopid]), and lipophilic
substances (probucol). Patients re-ceiving long-term therapy with these
medications require close medical supervision. Hypertension, which may
accelerate the rate at which atherosclerotic lesions form in high-pressure
vessels, can lead to cerebrovascular accident (CVA; brain attack, stroke),
is-chemic renal disease, severe peripheral arterial disease, or coronary artery
disease. Results of large, randomized studies demonstrated dramatic reductions
in myocardial infarction, stroke, and cardio-vascular death when blood pressure
was decreased to at least 140/90 mm Hg (Moser, 1999; McAlister et al., 2001).
Although
no single risk factor has been identified as the pri-mary contributor to the
development of atherosclerotic cardio-vascular disease, it is clear that the
greater the number of risk factors, the greater the likelihood of developing
the disease. Elim-ination of all controllable risk factors, particularly
tobacco use, is strongly recommended.
Clinical Manifestations
The
clinical signs and symptoms resulting from atherosclerosis depend on the organ
or tissue affected.
Medical Management
The
traditional medical management of atherosclerosis involves modification of risk
factors, a controlled exercise program to improve circulation and increase the
functioning capacity of the circulation, medication, and interventional or
surgical graft procedures.
SURGICAL MANAGEMENT
Vascular
surgical procedures are divided into two groups: inflow procedures, which
provide blood supply from the aorta into the femoral artery, and outflow
procedures, which provide blood supply to vessels below the
femoral artery. Inflow surgical procedures are discussed with diseases of the
aorta and outflow procedures with peripheral arterial occlusive disease.
RADIOLOGIC INTERVENTIONS
Several
interventional radiologic techniques are important ad-junctive therapies to
surgical procedures. If an isolated lesion or lesions are identified during the
arteriogram, angioplasty, also
called percutaneous transluminal angioplasty (PTA), may be per-formed. After
the patient receives a local anesthetic, a balloon-tipped catheter is
maneuvered across the area of stenosis. Exactly how PTA works is controversial.
Some theorize that it improves blood flow by overstretching (and thereby
dilating) the elastic fibers of the nondiseased arterial segment, but most
clinicians be-lieve that the procedure widens the arterial lumen by cracking
and flattening the plaque against the vessel wall . Com-plications from PTA
include hematoma formation, embolus, dissection
(separation of the intima) of the vessel, and bleeding.To decrease the risk
of reocclusion, stents (small, mesh tubes made of nitinol, titanium, or
stainless steel) may be inserted to support the walls of blood vessels and
prevent collapse immedi-ately after balloon inflation (Fig. 31-8). A variety of
covered wall stents and stent-grafts may be used for short-segment stenoses.
Complications associated with stent or stent-graft use include dis-tal
embolization, intimal damage (dissection), and dislodgment. The advantage of
angioplasty, stents, and stent-grafts is the de-creased length of hospital stay
required for the treatment; many of the procedures are performed on an
outpatient basis.
Related Topics