Chapter: Psychiatric Mental Health Nursing : Schizophrenia
Application of the Nursing Process: Assessment - Schizophrenia
APPLICATION OF THE NURSING
PROCESS
Assessment
Schizophrenia affects thought processes and content, per-ception,
emotion, behavior, and social functioning; how-ever, it affects each individual
differently. The degree of impairment in both the acute or psychotic phase and
the chronic or long-term phase varies greatly; thus, so do the needs of and the
nursing interventions for each affected client. The nurse must not make
assumptions about the client’s abilities or limitations based solely on the
medical diagnosis of schizophrenia.
For example, the nurse may care for a client in an acute inpatient
setting. The client may appear frightened, hear voices (hallucinate), make no
eye contact, and mumble con-stantly. The nurse would deal with the positive, or
psychotic, ![]()
![]() signs of the disease. Another nurse may
encounter a client with schizophrenia in a community setting who is not
expe-riencing psychotic symptoms; rather, this client lacks energy for daily
tasks and has feelings of loneliness and isolation (negative signs of
schizophrenia). Although both clients have the same medical diagnosis, the
approach and interventions that each nurse takes would be very different.
signs of the disease. Another nurse may
encounter a client with schizophrenia in a community setting who is not
expe-riencing psychotic symptoms; rather, this client lacks energy for daily
tasks and has feelings of loneliness and isolation (negative signs of
schizophrenia). Although both clients have the same medical diagnosis, the
approach and interventions that each nurse takes would be very different.
History
The nurse first elicits information about the client’s previous
history with schizophrenia to establish baseline data. He or she asks questions
about how the client functioned before the crisis developed, such as “How do
you usually spend your time?” and “Can you describe what you do each day?”
The nurse assesses the age at onset of schizophrenia, knowing that
poorer outcomes are associated with an ear-lier age at onset. Learning the
client’s previous history of hospital admissions and response to
hospitalization also is important.
The nurse also assesses the client for previous suicide attempts.
Ten percent of all people with schizophrenia even-tually commit suicide. The
nurse might ask, “Have you ever attempted suicide?” or “Have you ever heard
voices telling you to hurt yourself?” Likewise, it is important to elicit
information about any history of violence or aggression because a history of
aggressive behavior is a strong predictor of future aggression. The nurse might
ask, “What do you do when you are angry, frustrated, upset, or scared?”
The nurse assesses whether the client has been using current
support systems by asking the client or significant others the following
questions:
·
Has the client kept in contact with family or friends?
·
Has the client been to scheduled groups or therapy appointments?
·
Does the client seem to run out of money between paychecks?
·
Have the client’s living arrangements changed recently?
Finally, the nurse assesses the client’s perception of his or her
current situation—that is, what the client believes to be significant present
events or stressors. The nurse can gather such information by asking, “What do
you see as the primary problem now?” or “What do you need help managing now?”
General Appearance, Motor Behavior, and Speech
Appearance may vary widely among different clients with
schizophrenia. Some appear normal in terms of being dressed appropriately,
sitting in a chair conversing with the nurse and exhibiting no strange or
unusual postures or gestures. Others exhibit odd or bizarre behavior. They may
appear disheveled and unkempt with no obvious concern for their hygiene, or
they may wear strange or inappropri-ate clothing (for instance, a heavy wool
coat and stocking cap in hot weather).
Overall motor behavior also may appear odd. The cli-ent may be
restless and unable to sit still, exhibit agitationand pacing, or appear
unmoving (catatonia). He or she also
may demonstrate seemingly purposeless gestures (stereotypic behavior) and odd
facial expressions such as grimacing. The client may imitate the movements and
gestures of someone whom he or she is observing (echop-raxia). Rambling speech that may or may not make sense to the listener is likely to accompany
these behaviors.
Conversely, the client may exhibit psychomotor retar-dation (a general slowing of all movements).
Sometimes the client may be almost
immobile, curled into a ball (fetal position). Clients with the catatonic type
of schizophrenia can exhibit waxy flexibility: they maintain any position in which
they are placed, even if the position is awkward or uncomfortable.
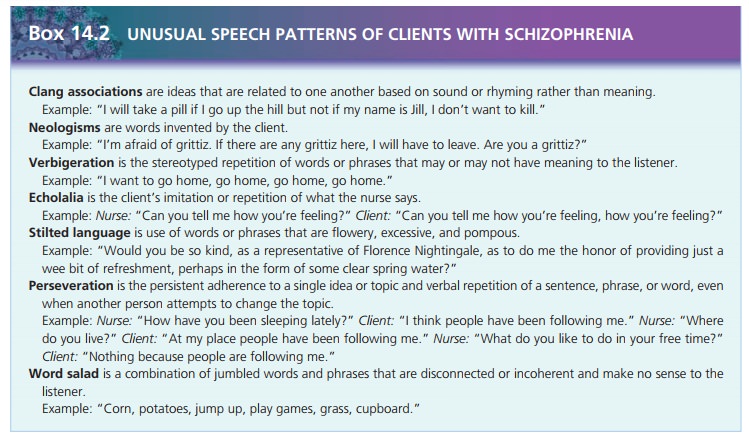
The client may exhibit an unusual speech pattern. Two typical
patterns are word salad (jumbled
words and phrases that are disconnected or incoherent and make no sense to the
listener) and echolalia (repetition
or imitation of what someone else says). Speech may be slowed or accelerated in
rate and volume: the client may speak in whispers or hushed tones or may talk
loudly or yell. Latency of response
refers to hesitation before the client responds to questions. This latency or
hesitation may last 30 or 45 seconds and usually indicates the client’s
difficulty with cognition or thought processes.
Mood and Affect
Clients with schizophrenia report and demonstrate wide variances in
mood and affect. They often are described as having flat affect (no facial expression) or blunted affect (few observable facial expressions). The typical
facial expression often is described as mask-like. The affect also may be
described as silly, characterized by giddy laughter for no apparent reason. The
client may exhibit an inap-propriate expression or emotions incongruent with
the context of the situation. This incongruence ranges from mild or subtle to
grossly inappropriate. For example, the client may laugh and grin while
describing the death of a family member or weep while talking about the
weather.
The client may report feeling depressed and having no pleasure or
joy in life (anhedonia). Conversely,
he or she may report feeling all-knowing, all-powerful, and not at all
concerned with the circumstance or situation. It is more common for the client
to report exaggerated feelings of well-being during episodes of psychotic or
delusional thinking and a lack of energy or pleasurable feelings dur-ing the
chronic, or long-term, phase of the illness.
Thought Process and Content
Schizophrenia often is referred to as a thought disorder because
that is the primary feature of the disease: thought processes become
disordered, and the continuity of thoughts and information processing is
disrupted. The nurse can assess thought process by inferring from what the
client says. He or she can assess thought content by evaluating what the client
actually says. For example, clients may suddenly stop talking in the middle of
a sentence and remain silent for several seconds to 1 minute (thought blocking). They also may state
that they believe others can hear their thoughts(thought broadcasting), that others are taking their thoughts (thought withdrawal), or that others are
placing thoughts in their mind against their will (thought insertion).
Clients also may exhibit tangential thinking, which is veering onto
unrelated topics and never answering the original question:
Nurse: “How have you been sleeping lately?”
Client: “Oh, I try to sleep at night. I like to listento music to help
me sleep. I really like country-western music best. What do you like? Can I
havesomething to eat pretty soon? I’m hungry.”
Nurse: “Can you tell me how you’ve been sleeping?
Circumstantiality may be evidenced if the client gives unnecessary
details or strays from the topic but eventually provides the requested
information:
Nurse: “How have you been sleeping lately?”
Client: “Oh, I go to bed early, so I can get plenty of rest. I like to
listen to music or read before bed. Right
now I’m reading
a good mystery. Maybe I’ll write
a mystery someday. Butit isn’t helping, reading I mean. I have been getting
only 2 or 3 hours of sleep at night.”
Poverty of content (alogia)
describes the lack of any real meaning or substance in what the client says:
Nurse: “How have you been sleeping lately?”
Client: “Well, I guess, I don’t know, hard to tell.”
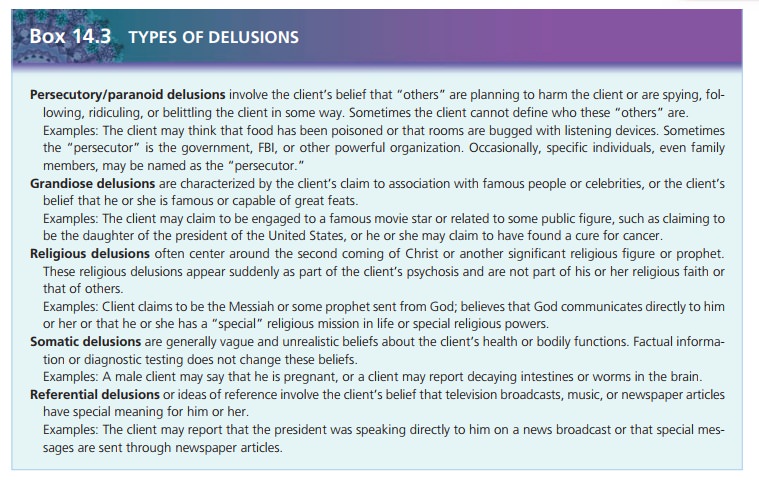
Delusions
Clients with schizophrenia usually experience delusions (fixed, false beliefs with no basis in reality) in the
psy-chotic phase of the illness. A common characteristic of schizophrenic
delusions is the direct, immediate, and total certainty with which the client
holds these beliefs. Because the client believes the delusion, he or she
therefore acts accordingly. For example, the client with delusions of
per-secution is probably suspicious, mistrustful, and guarded about disclosing
personal information; he or she may examine the room periodically or speak in
hushed, secre-tive tones.
The theme or content of the delusions may vary. External
contradictory information or facts can-not alter these delusional beliefs. If
asked why he or she believes such an unlikely idea, the client often replies, “I
just know it.”
Initially, the nurse assesses the content and depth of the delusion
to know what behaviors to expect and to try to establish reality for the
client. When eliciting information about the client’s delusional beliefs, the
nurse must be careful not to support or challenge them. The nurse might ask the
client to explain what he or she believes by saying “Please explain that to me”
or “Tell me what you’re think-ing about that.”
Sensorium and Intellectual Processes
One hallmark symptom of schizophrenic psychosis is hallucinations (false sensory
perceptions, or perceptual experiences
that do not exist in reality). Hallucinations can involve the five senses and
bodily sensations. They can be threatening and frightening for the client; less
frequently, clients report hallucinations as pleasant. Initially, the client
perceives hallucinations as real, but later in the illness, he or she may
recognize them as hallucinations.
Hallucinations are distinguished from illusions, which are misperceptions of actual environmental
stim-uli. For example, while walking through the woods, a person believes he
sees a snake at the side of the path. On closer examination, however, he
discovers it is only a curved stick. Reality or factual information corrected
this illusion. Hallucinations, however, have no such basis in reality.
The following are the various types of hallucinations (Kirkpatrick
& Tek, 2005):
Auditory hallucinations, the most common type,
involve hearing sounds, most often
voices, talking to or about the client. There may be one or multiple voices; a
famil-iar or unfamiliar person’s voice may be speaking. Com-mand hallucinations are voices demanding that the client take action, often to harm self
or others, and are considered dangerous.
·
Visual hallucinations involve seeing images that do
not exist at all, such as lights or a
dead person, or distortions such as seeing a frightening monster instead of the
nurse. They are the second most common type of hallucination.
·
Olfactory hallucinations involve smells or odors. They may be a specific scent such as urine
or feces or a more general scent such as a rotten or rancid odor. In addition
to clients with schizophrenia, this type of hallucination often occurs with
dementia, seizures, or cerebrovascu-lar accidents.
·
Tactile hallucinations refer to sensations such as
electric-ity running through the body or bugs crawling on the skin. Tactile
hallucinations are found most often in cli-ents undergoing alcohol withdrawal;
they rarely occur in clients with schizophrenia.
·
Gustatory hallucinations involve a taste lingering in
the mouth or the sense that food
tastes like something else. The taste may be metallic or bitter or may be
repre-sented as a specific taste.
·
Cenesthetic hallucinations involve the client’s report
that he or she feels bodily functions
that are usually unde-tectable. Examples would be the sensation of urine
forming or impulses being transmitted through the brain.
·
Kinesthetic hallucinations occur when the client is
mo-tionless but reports the sensation of bodily movement. Occasionally, the
bodily movement is something un-usual, such as floating above the ground.
During episodes of psychosis, clients are commonly disoriented to
time and sometimes place. The most extreme form of disorientation is depersonalization, in which the client
feels detached from her or his behavior. Although the client can state her or
his name correctly, she or he feels as if her or his body belongs to someone else
or that her or his spirit is detached from the body.
Assessing the intellectual processes of a client with schizophrenia
is difficult if he or she is experiencing psy-chosis. The client usually
demonstrates poor intellectual functioning as a result of disordered thoughts.
Neverthe-less, the nurse should not assume that the client has limited
intellectual capacity based on impaired thought processes. It may be that the
client cannot focus, concen-trate, or pay adequate attention to demonstrate his
or her intellectual abilities accurately. The nurse is more likely to obtain
accurate assessments of the client’s intellectual abil-ities when the client’s
thought processes are clearer.
Clients often have difficulty with abstract thinking and may
respond in a very literal way to other people and the environment. For example,
when asked to interpret the proverb, “A stitch in time saves nine,” the client
may explain it by saying, “I need to sew up my clothes.” The client may not
understand what is being said and can easily misinterpret instructions. This
can pose serious problems during medication administration. For example, the
nurse may tell the client, “It is always important to take all your
medications.” The client may misinterpret the nurse’s statement and take the
entire supply of medication at one time.
Judgment and Insight
Judgment is frequently impaired in the client with schizo-phrenia.
Because judgment is based on the ability to inter-pret the environment
correctly, it follows that the client with disordered thought processes and
environmental misinterpretations will have great difficulty with judg-ment. At
times, lack of judgment is so severe that clients cannot meet their needs for
safety and protection and place themselves in harm’s way. This difficulty may
range from failing to wear warm clothing in cold weather to failing to seek
medical care even when desperately ill. The client also may fail to recognize
needs for sleep or food.
Insight also can be severely impaired, especially early in the illness,
when the client, family, and friends do not understand what is happening. Over
time, some clients can learn about the illness, anticipate problems, and seek
appropriate assistance as needed. However, chronic diffi-culties result in
clients who fail to understand schizophre-nia as a long-term health problem
requiring consistent management.
Self-Concept
Deterioration of the concept of self is a major problem in
schizophrenia. The phrase loss of ego
boundaries describes the client’s lack of a clear sense of where his or her
own body, mind, and influence end and where those aspects of other animate and
inanimate objects begin. This lack of ego boundaries is evidenced by
depersonalization, dereal-ization (environmental objects become smaller or
larger or seem unfamiliar), and ideas of
reference. Clients may believe they are fused with another person or
object, may not recognize body parts as their own, or may fail to know whether
they are male or female. These difficulties are the source of many bizarre behaviors
such as public undress-ing or masturbating, speaking about oneself in the third
person, or physically clinging to objects in the environ-ment. Body image
distortion also may occur.
Roles and Relationships
Social isolation is prevalent in clients with schizophrenia, partly
as a result of positive signs such as delusions, hal-lucinations, and loss of
ego boundaries. Relating to others is difficult when one’s self-concept is not
clear. Clients also have problems with trust and intimacy, which interfere with
the ability to establish satisfactory relationships. Low self-esteem, one of
the negative signs of schizophrenia, further complicates the client’s ability
to interact with oth-ers and the environment. These clients lack confidence,
feel strange or different from other people, and do not believe they are
worthwhile. The result is avoidance of other people.
The client may experience great frustration in attempt-ing to
fulfill roles in the family and community. Success in school or at work can be
severely compromised because the client has difficulty thinking clearly,
remembering, paying attention, and concentrating. Subsequently, he or she lacks
motivation. Clients who develop schizophrenia at young ages have more
difficulties than those whose ill-ness developed later in life because they did
not have the opportunity to succeed in these areas before the illness.
Fulfilling family roles, such as that of son or daughter or
sibling, is difficult for these clients. Often, their erratic or unpredictable
behavior frightens or embarrasses family members, who become unsure what to
expect next. Fami-lies also may feel guilty or responsible, believing they
somehow failed to provide a loving supportive home life. These clients also may
believe they have disappointed their families because they cannot become
independent or successful.
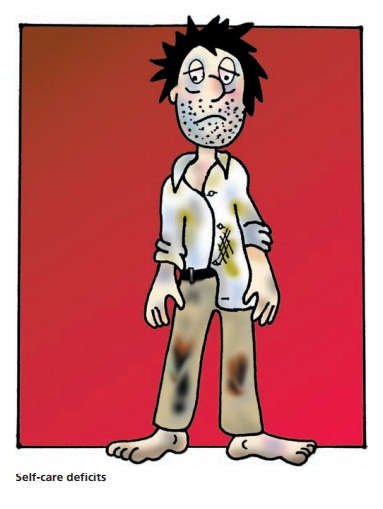
Physiologic and Self-Care Considerations
Clients with schizophrenia may have significant self-care deficits.
Inattention to hygiene and grooming needs is common, especially during psychotic
episodes. The client can become so preoccupied with delusions or
hallucina-tions that he or she fails to perform even basic activities of daily
living.
Clients also may fail to recognize sensations such as hunger or
thirst, and food or fluid intake may be inadequate. This can result in
malnourishment and constipation. Con-stipation is also a common side effect of
antipsychotic medications, compounding the problem. Paranoia or excessive fears
that food and fluids have been poisoned are common and may interfere with
eating. If the client is agi-tated and pacing, he or she may be unable to sit
down long enough to eat.
Occasionally, clients develop polydipsia
(excessive water intake), which leads to water intoxication. Serum sodium
levels can become dangerously low, leading to seizures. Polydipsia usually is
seen in clients who have had severe and persistent mental illness for many
years as well as long-term therapy with antipsychotic medications. It may be
caused by the behavioral state itself or may be precipitated by the use of
antidepressant or antipsychotic medications (Dundas, Harris, & Narasimhan,
2007). Sleep problems are common. Hallucinations may stimulate clients,
resulting in insomnia. Other times, clients are suspicious and believe harm will
come to them if they sleep. As in other self-care areas, the client may not
correctly perceive or acknowledge physical cues such as fatigue.
To assist the client with community living, the nurse assesses
daily living skills and functional abilities. Such skills—having a bank account
and paying bills, buying food and preparing meals, and using public
transportation—are often difficult tasks for the client with schizophrenia. He
or she might never have learned such skills or may be unable to accomplish them
consistently.
Related Topics