Chapter: Psychiatric Mental Health Nursing : Eating Disorders
Application of the Nursing Process - Eating Disorders
APPLICATION OF THE NURSING
PROCESS
Although anorexia and bulimia have several differences, many
similarities are found in assessing, planning, implementing, and evaluating
nursing care for clients with these disorders. Thus, this section addresses
both eating disorders and highlights differences where they exist.
Assessment
Several specialized tests have been developed for eating disorders.
An assessment tool such as the Eating Attitudes Test often is used in studies
of anorexia and bulimia. This test also can be used at the end of treatment to
evaluate outcomes because it is sensitive to clinical changes.
History
Family members often describe clients with anorexia nervosa as
perfectionists with above-average intelligence, achieve-ment oriented,
dependable, eager to please, and seeking approval before their condition began.
Parents describe cli-ents as being “good, causing us no trouble” until the
onset of anorexia. Likewise, clients with bulimia often are focused on pleasing
others and avoiding conflict. Clients with bulimia, however, often have a
history of impulsive behavior such as substance abuse and shoplifting as well
as anxiety, depres-sion, and personality disorders (Schultz & Videbeck,
2009).
General Appearance and Motor Behavior
Clients with anorexia appear slow, lethargic, and fatigued; they
may be emaciated, depending on the amount of weightloss. They may be slow to
respond to questions and have difficulty deciding what to say. They are often
reluctant to answer questions fully because they do not want to acknowledge any
problem. They often wear loose-fitting clothes in layers, regardless of the
weather, both to hide weight loss and to keep warm (clients with anorexia are
generally cold). Eye contact may be limited. Clients may turn away from the
nurse, indicating their unwillingness to discuss problems or to enter
treatment.
Clients with bulimia may be underweight or overweight but are
generally close to expected body weight for age and size. General appearance is
not unusual, and they appear open and willing to talk.
Mood and Affect
Clients with eating disorders have labile moods that usu-ally
correspond to their eating or dieting behaviors. Avoid-ing “bad” or fattening
foods gives them a sense of power and control over their bodies, whereas
eating, binging, or purging leads to anxiety, depression, and feeling out of
control. Clients with eating disorders often seem sad, anx-ious, and worried.
Those with anorexia seldom smile, laugh, or enjoy any attempts at humor; they
are somber ![]()
![]() and serious most of the time. In contrast,
clients with buli-mia are initially pleasant and cheerful as though nothing is
wrong. The pleasant façade usually disappears when they begin describing binge
eating and purging; they may express intense guilt, shame, and embarrassment.
and serious most of the time. In contrast,
clients with buli-mia are initially pleasant and cheerful as though nothing is
wrong. The pleasant façade usually disappears when they begin describing binge
eating and purging; they may express intense guilt, shame, and embarrassment.
It is important to ask clients with eating disorders about thoughts
of self-harm or suicide. It is not uncommon for these clients to engage in
self-mutilating behaviors, such as cutting. Concern about self-harm and
suicidal behavior should increase when clients have a history of sexual abuse.
Thought Processes and Content
Clients with eating disorders spend most of the time think-ing
about dieting, food, and food-related behavior. They are preoccupied with their
attempts to avoid eating or eat-ing “bad” or “wrong” foods. Clients cannot
think about themselves without thinking about weight and food. The body image
disturbance can be almost delusional; even if clients are severely underweight,
they can point to areas on their buttocks or thighs that are “still fat,”
thereby fuel-ing their need to continue dieting. Clients with anorexia who are
severely underweight may have paranoid ideas about their family and health care
professionals, believing they are their “enemies” who are trying to make them
fat by forcing them to eat.
Sensorium and Intellectual Processes
Generally, clients with eating disorders are alert and ori-ented;
their intellectual functions are intact. The exception is clients with anorexia
who are severely malnourished and showing signs of starvation, such as mild
confusion, slowed mental processes, and difficulty with concentration and
attention.
Judgment and Insight
Clients with anorexia have very limited insight and poor judgment
about their health status. They do not believe they have a problem; rather,
they believe others are trying to interfere with their ability to lose weight
and to achieve the desired body image. Facts about failing health status are
not enough to convince these clients of their true problems. Clients with
anorexia continue to restrict food intake or to engage in purging despite the
negative effect on health.
In contrast, clients with bulimia are ashamed of the binge eating
and purging. They recognize these behaviors as abnormal and go to great lengths
to hide them. They feel out of control and unable to change even though they
recognize their behaviors as pathologic.
Self-Concept
Low self-esteem is prominent in clients with eating dis-orders.
They see themselves only in terms of their ability to control their food intake
and weight. They tend to judge themselves harshly and see themselves as “bad”
if they eat certain foods or fail to lose weight. They overlook or ignore other
personal characteristics or achievements as less important than thinness.
Clients often perceive themselves as helpless, powerless, and ineffective. This
feeling of lack of control over themselves and their envi-ronment only
strengthens their desire to control their weight.
Roles and Relationships
Eating disorders interfere with the ability to fulfill roles and to
have satisfying relationships. Clients with anorexia may begin to fail at
school, which is in sharp contrast to previously successful academic
performance. They with-draw from peers and pay little attention to friendships.
They believe that others will not understand or fear they will begin
out-of-control eating with others.
Clients with bulimia feel great shame about their binge eating and
purging behaviors. As a result, they tend to lead secret lives that include
sneaking behind the backs of friends and family to binge and purge in privacy.
The time spent buying and eating food and then purging can inter-fere with role
performance both at home and at work.
Physiologic and Self-Care Considerations
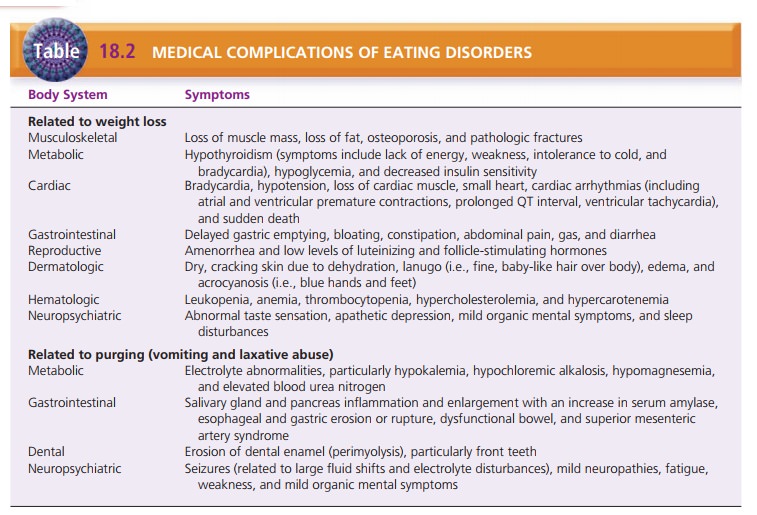
The health status of clients with eating disorders relates directly
to the severity of self-starvation, purging behav-iors, or both (see Table
18.2). In addition, clients may exercise excessively, almost to the point of
exhaustion, in an effort to control weight. Many clients have sleep
distur-bances such as insomnia, reduced sleep time, and early-morning wakening.
Those who frequently vomit have many dental problems, such as loss of tooth
enamel, chipped and ragged teeth, and dental caries. Frequent vomiting also may
result in mouth sores. Complete medi-cal and dental examinations are essential.
Data Analysis
Nursing diagnoses for clients with eating disorders include the
following:
·
Imbalanced Nutrition: Less Than/More Than Body Requirements
·
Ineffective Coping
·
Disturbed Body Image
·
Chronic Low Self-esteem
Other nursing diagnoses may be pertinent, such as Defi-cient Fluid
Volume, Constipation, Fatigue, and Activity Intolerance.
Outcome Identification
For severely malnourished clients, their medical condition must be
stabilized before psychiatric treatment can begin. Medical stabilization may
include parenteral fluids, total parenteral nutrition, and cardiac monitoring.
![]()
![]() Examples of expected outcomes for clients with
eating disorders include the following:
Examples of expected outcomes for clients with
eating disorders include the following:
·
The client will establish adequate nutritional eating patterns.
·
The client will eliminate use of compensatory behaviors such as
excessive exercise and use of laxatives and diuretics.
·
The client will demonstrate coping mechanisms not related to food.
·
The client will verbalize feelings of guilt, anger, anxiety, or an
excessive need for control.
·
The client will verbalize acceptance of body image with stable body
weight.
Interventions
Establishing Nutritional Eating Patterns
Typically, inpatient treatment is for clients with anorexia
ner-vosa who are severely malnourished and clients with bulimia whose binge
eating and purging behaviors are out of control. Primary nursing roles are to
implement and to supervise the regimen for nutritional rehabilitation. Total
parenteral nutri-tion or enteral feedings may be prescribed initially when a
client’s health status is severely compromised.
When clients can eat, a diet of 1,200 to 1,500 calories per day is
ordered, with gradual increases in calories until clients are ingesting
adequate amounts for height, activity level, and growth needs. Typically,
allotted calories are divided into three meals and three snacks. A liquid
protein supplement is given to replace any food not eaten to ensure consumption
of the total number of prescribed calories. The nurse is responsible for
monitoring meals and snacks and often initially will sit with a client during
eating at a table away from other clients. Depending on the treatment program,
diet beverages and food substitutions may be prohibited, and a specified time
may be set for consuming each meal or snack. Clients also may be discouraged
from performing food rituals such as cutting food into tiny pieces or mixing
food in unusual combinations. The nurse must be alert for any attempts by
clients to hide or to dis-card food.
After each meal or snack, clients may be required to remain in view
of staff for 1 to 2 hours to ensure they do not empty the stomach by vomiting.
Some treatment pro-grams limit client access to bathrooms without supervi-sion,
particularly after meals, to discourage vomiting. As clients begin to gain
weight and to become more indepen-dent in eating behavior, these restrictions are
reduced gradually.
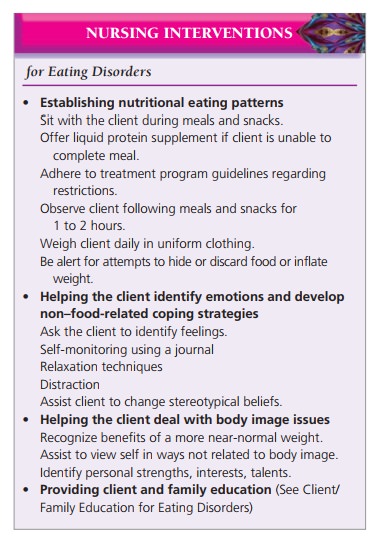
In most treatment programs, clients are weighed only once daily,
usually on awakening and after they have emp-tied the bladder. Clients should
wear minimal clothing, such as a hospital gown, each time they are weighed.
They may attempt to place objects in their clothing to give the appearance of
weight gain.
Clients with bulimia often are treated on an outpatient basis. The
nurse must work closely with clients to estab-lish normal eating patterns and
to interrupt the binge and purge cycle. He or she encourages clients to eat
meals with their families or, if they live alone, with friends. Clients always
should sit at a table in a designated eating area such as a kitchen or dining
room. It is easier for clients to follow a nutritious eating plan if it is
written in advance and gro-ceries are purchased for the planned menus. Clients
must avoid buying foods frequently consumed during binges, such as cookies,
candy bars, and potato chips. They should discard or move to the kitchen food that
was kept at work, in the car, or in the bedroom.
Identifying Emotions and Developing Coping Strategies
Because clients with anorexia have problems with self-awareness,
they often have difficulty identifying and expressing feelings (alexithymia). Therefore, they often
express these feelings in terms of somatic complaints such as feeling fat or
bloated. The nurse can help clients begin to recognize emotions such as anxiety
or guilt by asking them to describe how they are feeling and allowing ade-quate
time for response. The nurse should not ask, “Are you sad?” or “Are you
anxious?” because a client may quickly agree rather than struggle for an
answer. The nurse encourages the client to describe her or his feelings. This
approach can eventually help clients to recognize their emotions and to connect
them to their eating behaviors.
Self-monitoring is a cognitive–behavioral
technique designed to help clients
with bulimia. It may help clients to identify behavior patterns and then
implement tech-niques to avoid or to replace them (Schmidt, 2008).
Self-monitoring techniques raise client awareness about behavior and help them
to regain a sense of control. The nurse encourages clients to keep a diary of
all food eaten throughout the day, including binges, and to record moods,
emotions, thoughts, circumstances, and interactions sur-rounding eating and
binging or purging episodes. In this way, clients begin to see connections
between emotions and situations and eating behaviors. The nurse can then help
clients to develop ways to manage emotions such as anxiety by using relaxation
techniques or distraction with music or another activity. This is an important
step toward helping clients find ways to cope with people, emotions, or
situations that do not involve food.
Dealing with Body Image Issues
The nurse can help clients to accept a more normal body image. This
may involve clients agreeing to weigh more than they would like, to be healthy,
and to stay out of the hospital. When clients experience relief from emotional
distress, have increased self-esteem, and can meet their emotional needs in
healthy ways, they are more likely to accept their weight and body image.
The nurse also can help clients to view themselves in terms other
than weight, size, shape, and satisfaction with body image. Helping clients to
identify areas of personal strength that are not food related broadens clients’
percep-tions of themselves. This includes identifying talents, interests, and
positive aspects of character unrelated to body shape or size.
Providing Client and Family Education
One primary nursing role in caring for clients with eating
disorders is providing education to help them take control of nutritional
requirements independently. This teaching can be done in the inpatient setting
during discharge plan-ning or in the outpatient setting. The nurse provides
extensive teaching about basic nutritional needs and the effects of restrictive
eating, dieting, and the binge and purge cycle. Clients need encouragement to
set realistic goals for eating throughout the day (Sylvester & Forman,
2008). Eating only salads and vegetables during the day may set up clients for
later binges as a result of too little dietary fat and carbohydrates.
For clients who purge, the most important goal is to stop. Teaching
should include information about the harmful effects of purging by vomiting and
laxative abuse. The nurse explains that purging is an ineffective means of
weight control and only disrupts the neuroendocrine system. In addition,
purging promotes binge eating by decreasing the anxiety that follows the binge.
The nurse ![]()
![]() explains that if clients can avoid purging,
they may be less likely to engage in binge eating. The nurse also teaches the
techniques of distraction and delay because they are useful against both
binging and purging. The longer clients can delay either binging or purging,
the less likely they are to carry out the behavior.
explains that if clients can avoid purging,
they may be less likely to engage in binge eating. The nurse also teaches the
techniques of distraction and delay because they are useful against both
binging and purging. The longer clients can delay either binging or purging,
the less likely they are to carry out the behavior.
The nurse explains to family and friends that they can be most
helpful by providing emotional support, love, and attention. They can express
concern about the client’s health, but it is rarely helpful to focus on food
intake, calo-ries, and weight.
Evaluation
The nurse can use assessment tools such as the Eating Attitudes
Test to detect improvement for clients with eat-ing disorders. Both anorexia
and bulimia are chronic for many clients. Residual symptoms such as dieting,
compul-sive exercising, and experiencing discomfort when eating in a social
setting are common. Treatment is considered successful if the client maintains
a body weight within 5% to 10% of normal with no medical complications from
starvation or purging.
Related Topics