Chapter: Essentials of Anatomy and Physiology: Lymphatic System and Immunity
Antibody-mediated immunity
Antibody-mediated immunity
Exposure of the body to an antigen can lead to the activation of B cells and the production of antibodies. The antibodies bind to the antigens, which can be destroyed through several different mechanisms. Because antibodies are in body fluids, antibody-mediated immunity is effective against extracellular antigens, such as bacteria, viruses (when they are outside cells), and toxins. Antibody-mediated immunity is also involved in certain allergic reactions.
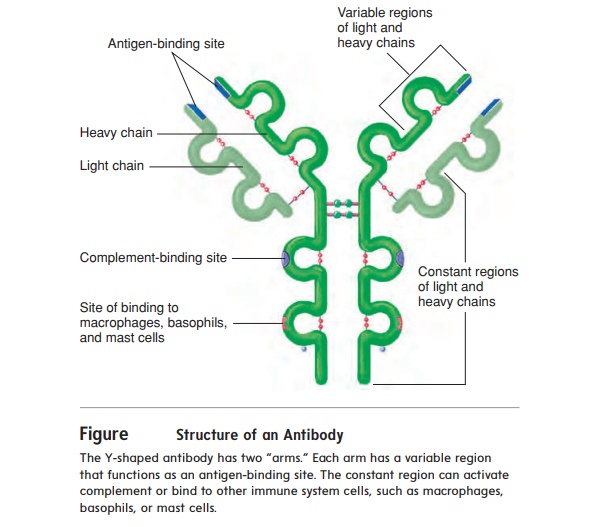
Structure of Antibodies
Antibodies are proteins produced in response to an antigen. They are Y-shaped molecules consisting of four polypeptide chains: two identical heavy chains and two identical light chains (figure 14.12). The end of each “arm” of the antibody is the variable region, the part of the antibody that combines with the antigen. The variable region of a particular antibody can join only with a particular antigen; this is similar to the lock-and-key model of enzymes. The rest of the antibody is the constant region, and it has several functions. For example, the constant region can activate complement, or it can attach the antibody to cells, such as macrophages, basophils, and mast cells.

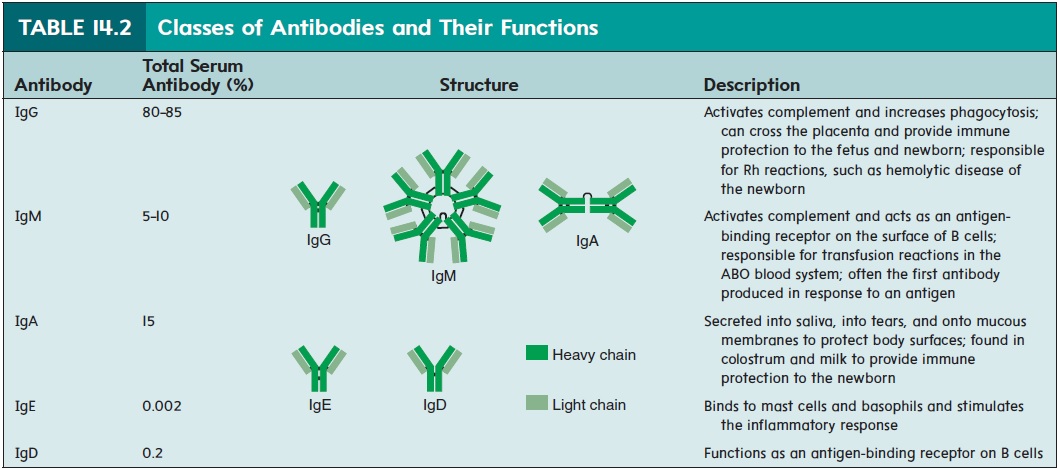
Antibodies make up a large portion of the proteins in plasma. Most plasma proteins can be separated into albumin and alpha, beta, and gamma globulin portions . Antibodies are sometimes called gamma globulins (glob′ ū-linz), because they are found mostly in the gamma globulin part of plasma, or immunoglobulins (Ig), because they are globulin proteins involved in immunity. The five general classes of antibodies are denoted IgG, IgM, IgA, IgE, and IgD (table 14.2).
Effects of Antibodies
Antibodies can affect antigens either directly or indirectly. Direct effects occur when a single antibody binds to an antigen and inactivates the antigen, or when many antigens are bound togetherand are inactivated by many antibodies (figure 14.13a,b). The ability of antibodies to join antigens together is the basis for many clinical tests, such as blood typing, because when enough antigens are bound together, they form visible clumps.
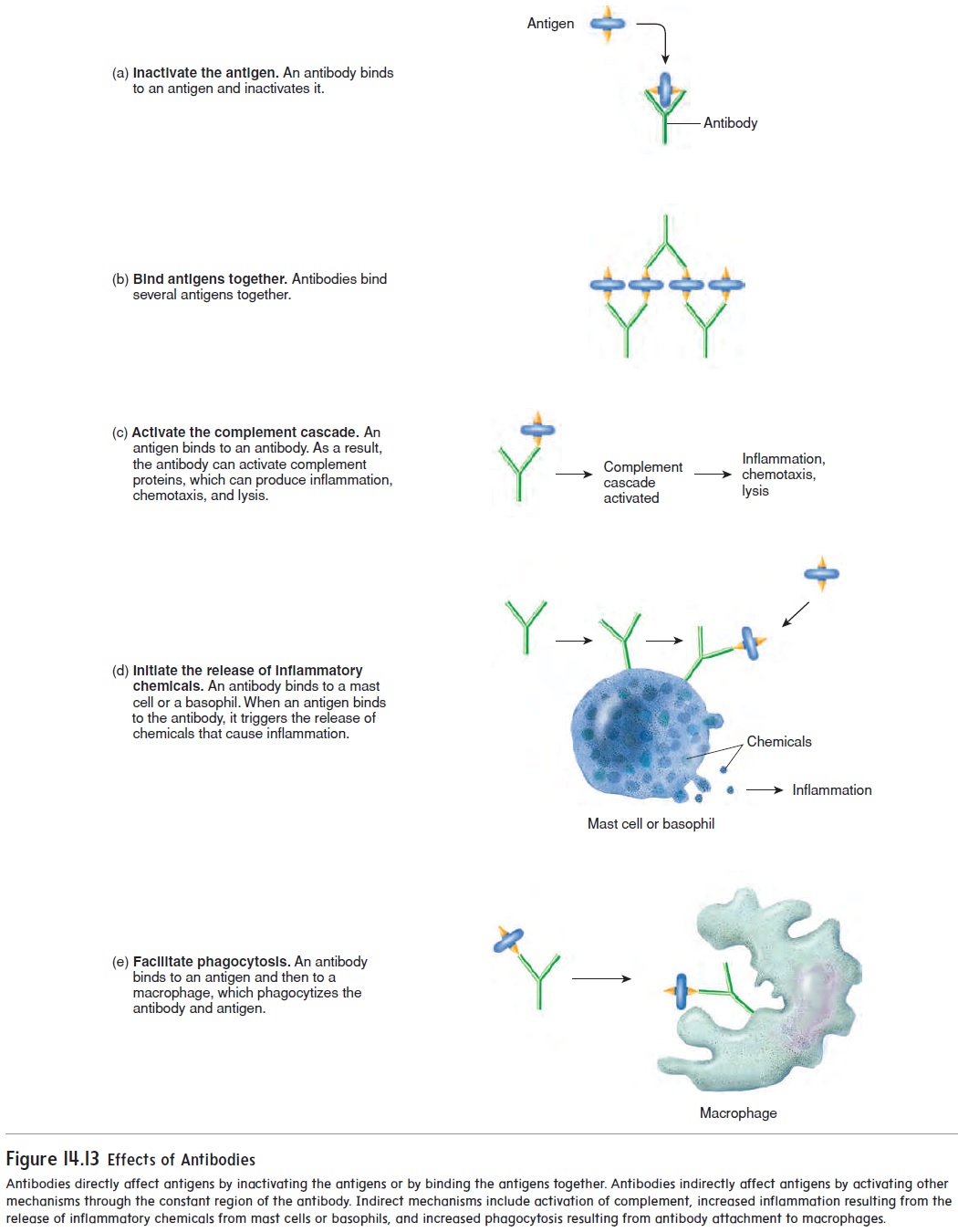
Most of the effectiveness of antibodies results from indirect effects (figure 14.13c–e). After an antibody has attached by its variable region to an antigen, the constant region of the antibody can activate other mechanisms that destroy the antigen. For exam-ple, the constant region of antibodies can activate complement, which stimulates inflammation, attracts white blood cells through chemotaxis, and lyses bacteria. When an antigen combines with the antibody, the constant region triggers the release of inflammatory chemicals from mast cells and basophils. For example, people who have hay fever inhale the antigens (usually plant pollens), which are then absorbed through the respiratory mucous mem-brane. The combination of the antigen with antibodies stimulates mast cells to release inflammatory chemicals, such as histamine. The resulting localized inflammatory response produces swell-ing and excess mucus production in the respiratory tract. Finally, macrophages can attach to the constant region of the antibody and phagocytize both the antibody and the antigen.
Antibody Production
The production of antibodies after the first exposure to an antigen is different from that following a second or subsequent exposure. The primary response results from the first exposure of a B cell to an antigen (figure 14.14, step 1). When the antigen binds to the antigen-binding receptor on the B cell and the B cell has been activated by a helper T cell, the B cell undergoes sev-eral divisions to form plasma cells and memory B cells. Plasma cells produce antibodies. The primary response normally takes 3–14 days to produce enough antibodies to be effective against the antigen. In the meantime, the individual usually develops disease symptoms because the antigen has had time to cause tissue damage.
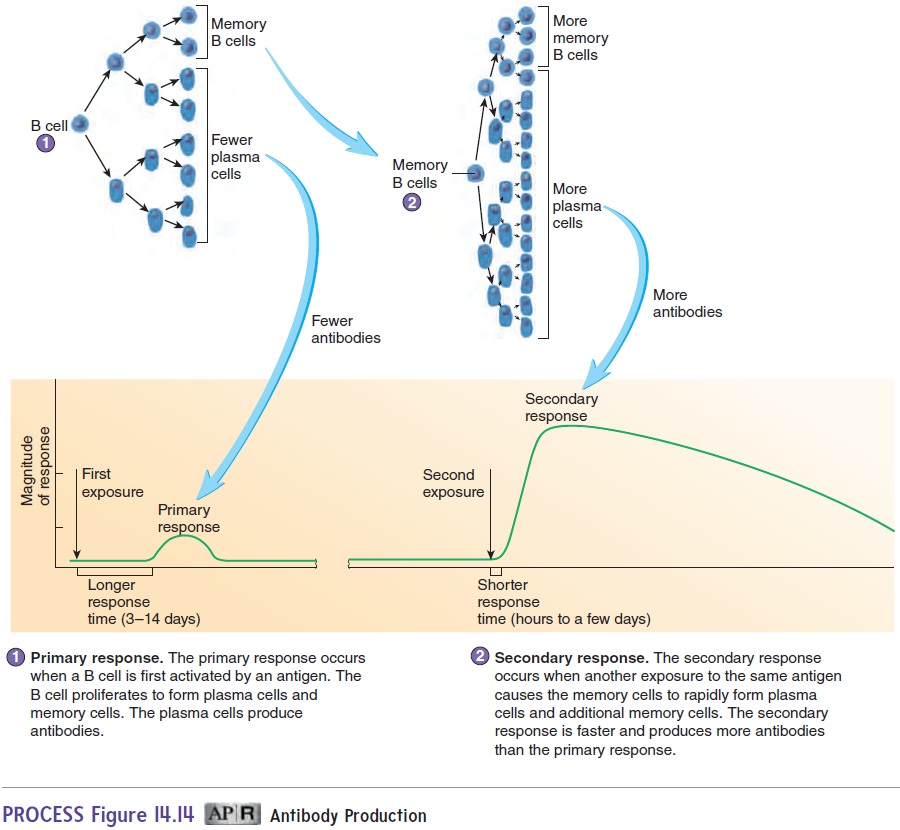
Memory B cells are responsible for the secondary response, or memory response, which occurs when the immune system is exposed to an antigen against which it has already produced a pri-mary response (figure 14.14, step 2). When exposed to the antigen, the memory B cells quickly divide to form plasma cells, which rapidly produce antibodies. The secondary response provides better protection than the primary response for two reasons: (1) The time required to start producing antibodies is less (hours to a few days), and (2) more plasma cells and antibodies are produced. As a con-sequence, the antigen is quickly destroyed, no disease symptoms develop, and the person is immune.
The secondary response also includes the formation of new memory cells, which provide protection against additional expo-sures to a specific antigen. Memory cells are the basis of adaptive immunity. After destruction of the antigen, plasma cells die, the antibodies they released are degraded, and antibody levels decline to the point where they can no longer provide adequate protection. However, memory cells persist for many years—for life, in some cases. If memory cell production is not stimulated, or if the memory cells produced are short-lived, it is possible to have repeated infec-tions of the same disease. For example, the same cold virus can cause the common cold more than once in the same person.
Related Topics