Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Patients with Endocrine Disease
Anesthesia for Obesity
Obesity
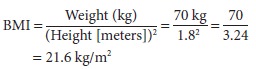
Overweight and obesity are classified using the body mass index (BMI).
Overweight is defined as a BMI of 24 kg/m2 or higher, obesity as a BMI of
30 or higher, and extreme obesity (formerly termed “morbid obesity”) as a BMI
of more than 40. BMI is calculated by dividing the weight (in kilo-grams) by
the height (in meters) squared. Health risks increase with the degree of
obesity and with increased abdominal distribution of weight. Men with a waist
measurement of 40 in. or more and women with a waist measurement of 35 in. or
more are at increased health risk. For a patient 1.8 m tall and weighing 70 kg,
the BMI would be as shown in the following formula:
Clinical Manifestations
Obesity is associated with many diseases,
includ-ing type 2 diabetes mellitus, hypertension, coronary artery disease,
obstructive sleep apnea, degenera-tive joint disease (osteoarthritis), and
cholelithiasis. Even in the absence of obvious coexisting disease, however,
extreme obesity has profound physiologi-cal consequences. Oxygen demand, CO2 production, and alveolar ventilation are
elevated because meta-bolic rate is proportional to body weight. Excessive
adipose tissue over the thorax decreases chest wall compliance even though lung
compliance may remain normal. Increased abdominal mass forces the diaphragm
cephalad, yielding lung volumes suggestive of restrictive lung disease.
Reductions in lung volumes are accentuated by the supine and Trendelenburg
positions. In particular, functional residual capacity may fall below closing
capacity. If this occurs, some alveoli will close during normal tidal volume
ventilation, causing a ventilation/per-fusion mismatch.
Whereas obese patients are often hypoxemic, only a few are hypercapnic,
which should be a warning of impending complications. Obesity-hypoventilation
syndrome, or obstructive sleep apnea (OSA), is a complication of extreme
obesity characterized by hypercapnia, cyanosis-induced polycythemia,
right-sided heart failure, and som-nolence. These patients appear to have blunted
respiratory drive and often suffer from loud snoring and upper-airway
obstruction during sleep. OSA patients often report dry mouths and daytime
som-nolence; bed partners frequently describe apneic pauses. OSA has also been
associated with increased perioperative complications including hyperten-sion,
hypoxia, arrhythmias, myocardial infarction, pulmonary edema, stroke, and
death. The potential for difficult mask ventilation and difficult intuba-tion,
followed by upper airway obstruction during recovery, should be anticipated.
OSA patients are vulnerable during the
postop-erative period, particularly when sedatives or opi-oids have been given.
When OSA patients are placed supine, the upper airway is even more prone to
obstruction. For patients with known or suspected OSA, postoperative continuous
positive airway pres-sure (CPAP) should be considered until the
anesthe-siologist can be sure that the patient can protect his or her airway
and maintain spontaneous ventilation without evidence of obstruction. Both the
American Society of Anesthesiologists and the Society of Ambulatory Anesthesia
offer guidelines on periop-erative management of the patient with OSA.
An OSA patient’s heart has an increased work-load, as cardiac output and
blood volume rise to perfuse additional fat stores. The elevation in cardiac
output (0.1 L/min/kg of adipose tissue) is achieved through an increase in
stroke volume—as opposed to heart rate. Arterial hypertension leads to left
ven-tricular hypertrophy. Elevations in pulmonary blood flow and pulmonary
artery vasoconstriction from persistent hypoxia can lead to pulmonary
hyperten-sion and cor pulmonale.
Obesity is also associated with gastrointestinal pathophysiology,
including hiatal hernia, gastro-esophageal reflux disease, delayed gastric
empty-ing, and hyperacidic gastric fluid, as well as with an increased risk of
gastric cancer. Fatty infiltration of the liver also occurs and may be
associated with abnormal liver tests, but the extent of infiltration does not
correlate well with the degree of liver test abnormality.
Anesthetic Considerations
A. Preoperative
For the reasons outlined above, obese patients are at an increased risk
for developing aspiration pneumo-nia. Pretreatment with H 2
antagonists and metoclo-pramide should be considered. Premedication with
respiratory depressant drugs must be avoided in patients with OSA.
Preoperative evaluation of extremely obese
patients undergoing major surgery should attempt to assess cardiopulmonary
reserve. Preoperative testing may include such items as chest radiograph, ECG,
and arterial blood gas analysis. Physical signs of cardiac failure (eg, sacral
edema) may be difficult to identify. Blood pressures must be taken with a cuff
of the appropriate size. Potential sites for intrave-nous and intraarterial
access should be checked in anticipation of technical difficulties. Obscured
land-marks, difficult positioning, and extensive layers of adipose tissue may make
regional
anesthe-sia difficult with standard equipment
and techniques. Obese patients may be difficult to intubate as a result of
limited mobility of thetemporomandibular and atlantooccipital joints, a
narrowed upper airway, and a shortened distance between the mandible and
sternal fat pads.
B. Intraoperative
Because of the risks of aspiration and hypoventilation, morbidly obese
patients are usually intubated for all but short general anesthetics. If
intubation appears likely to be difficult, the use of a fiberoptic
bron-choscope or video laryngoscopy is recommended. Positioning the patient on
an intubating ramp is help-ful. Auscultation of breath sounds may prove
difficult. Even controlled ventilation may require relatively increased
inspired oxygen concentrations to prevent hypoxia, particularly in the
lithotomy, Trendelenburg, or prone positions. Subdiaphragmatic abdominal
laparotomy packs can cause further deterioration of pulmonary function and a
reduction of arterial blood pressure by increasing the resistance to venous
return. Volatile anesthetics may be metabolized more exten-sively in obese
patients. Increased metabolism may explain the increased incidence of halothane
hepatitis observed in obese patients. Obesity has little clinical effect on the
rate of decline of alveolar anesthetic con-centrations and wake-up time, even
following long surgical procedures.
Theoretically, greater fat stores would
increase the volume of distribution for lipid-soluble drugs (eg,
benzodiazepines, opioids) relative to a lean per-son of the same body weight.
However, the volume of distribution of, for example, fentanyl or sufentanil is
so large that obesity has minimal influence. Water-soluble drugs (eg, NMBs)
have a much smaller vol-ume of distribution, which is minimally increased by
body fat. Nonetheless, the dosing of water-soluble drugs should be based on
ideal body weight to avoid overdosing. In reality, of course, clinical practice
does not always validate these expectations.
Although dosage requirements for epidural and
spinal anesthesia are difficult to predict, obese patients typically require
20–25% less local anes-thetic per blocked segment because of epidural fat and
distended epidural veins. Continuous epi-dural anesthesia has the advantage of
providing pain relief and the potential for decreasing respi-ratory
complications in the postoperative period. Regional nerve blocks, when
appropriate for the surgery, have the additional advantages of not inter-fering
with the postoperative deep vein thrombosis prophylaxis, rarely producing
hypotension, and of reducing the need for opioids.
C. Postoperative
Respiratory failure is a major postoperative
problem of morbidly obese patients. The risk of postopera-tive hypoxia is
increased in patients with preopera-tive hypoxia, following surgery involving
the thorax or upper abdomen (particularly vertical incisions). Extubation
should be delayed until the effects of NMBs are completely reversed and the
patient is awake. An obese patient should remain intubated until there is no
doubt that an adequate airway and tidal volume will be maintained. This does not mean that all obese patients need be
ventilated overnight in an intensive care unit. If the patient is extubated in
the operating room, supplemental oxygen should be provided during
transportation to the postan-esthesia care unit. A 45° modified sitting
position will improve ventilation and oxygenation. The risk of hypoxia extends
for several days into the postop-erative period, and providing supplemental
oxygen or CPAP, or both, should be routinely considered. Other common
postoperative complications in obese patients include wound infection, deep
venous thrombosis, and pulmonary embolism. Morbidly obese and OSA patients may
be candidates for out-patient surgery provided they are adequately moni-tored
and assessed postoperatively before discharge to home, and provided the
surgical procedure will not require large doses of opioids for postoperative
pain control.
Related Topics