Chapter: Clinical Anesthesiology: Anesthetic Management: Anesthesia for Genitourinary Surgery
Anesthesia for Cystoscopy
CYSTOSCOPY
Preoperative Considerations
Cystoscopy is the most commonly performed uro-logical procedure,
and indications for this investi-gative or therapeutic operation include
hematuria, recurrent urinary infections, renal calculi, and urinary
obstruction. Bladder biopsies, retrograde pyelograms, transurethral resection
of bladder tumors, extraction or laser lithotripsy of renal stones, and
placement or manipulation of ureteral catheters (stents) are also commonly
performed through the cystoscope.
Anesthetic management varies with the age and gender of the
patient and the purpose of the procedure. General anesthesia is usually
necessary for children. Viscous lidocaine topical anesthesia with or without
sedation is satisfactory for diag-nostic studies in most women because of the
short urethra. Operative cystoscopies involving biopsies, cauterization, or
manipulation of ureteral catheters require regional or general anesthesia. Many
men prefer regional or general anesthesia even for diag-nostic cystoscopy.
Intraoperative Considerations
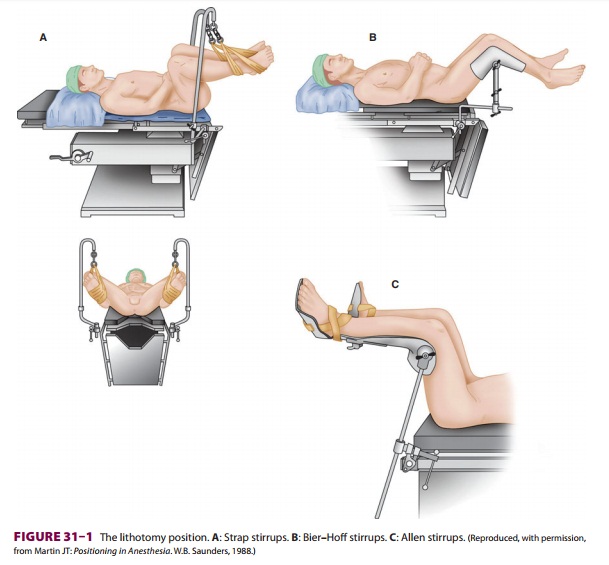
A. Lithotomy Position
Next to the supine position, the
lithotomy position is the most commonly used positionfor patients undergoing
urological and gynecologi-cal procedures. Failure to properly position and pad
the patient can result in pressure sores, nerve inju-ries, or compartment
syndromes. Two people are needed to safely move the patient’s legs simultane-ously
up into, or down from, the lithotomy position. Straps around the ankles or
special holders support the legs in lithotomy position ( Figure 31–1).
The leg supports should be padded wherever there is leg or foot contact, and
straps must not impede circula-tion. When the patient’s arms are tucked to the
side, caution must be exercised to prevent the fingers from being caught
between the mid and lower sec-tions of the operating room table when the lower
section is lowered and raised—many clinicians com-pletely encase the patient’s
hands and fingers with
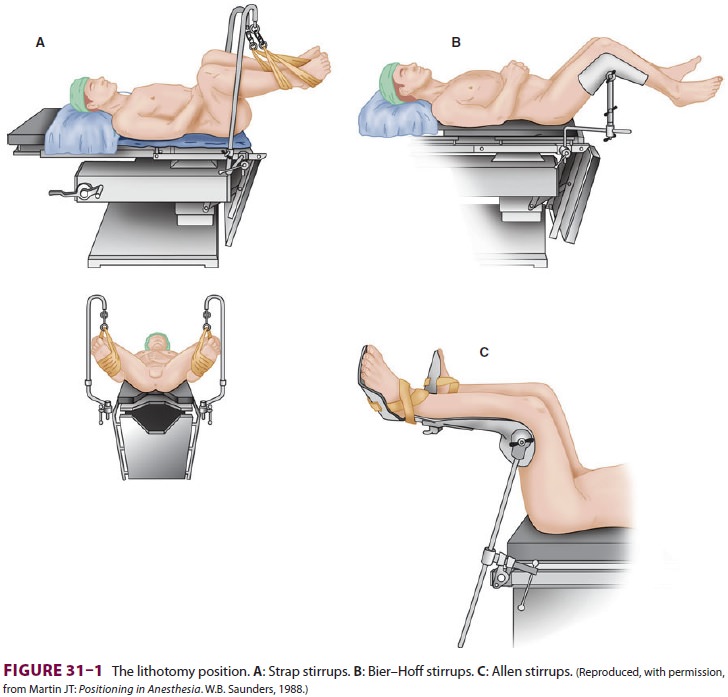
protective padding to minimize this
risk. Injury to the tibial (common peroneal) nerve, resulting in loss of
dorsiflexion of the foot, may result if the lateral knee rests against the
strap support. If the legs are allowed to rest on medially placed strap
supports, compression of the saphenous nerve can result in numbness along the
medial calf. Excessive flexion of the thigh against the groin can injure the
obturator and, less commonly, the femoral nerves. Extreme flexion at the thigh
can also stretch the sciatic nerve. The most common nerve injuries directly
associated with the lithotomy position involve the lumbosacral plexus. Brachial
plexus injuries can likewise occur if the upper extremities are inappropriately
positioned (eg, hyperextension at the axilla). Compartment syndrome of the
lower extremities with rhabdomy-olysis has been reported with prolonged time in
the lithotomy position, after which lower extremity nerve damage is also more
likely.
The lithotomy position is associated
with major physiological alterations. Functionalresidual capacity decreases, predisposing patientsto
atelectasis and hypoxia. This effect is amplified by steep Trendelenburg
positioning (>30°), which is commonly utilized in
combination with the lithot-omy position. Elevation of the legs drains blood
into the central circulation acutely and may thereby exacerbate congestive
heart failure (or treat a rela-tive hypovolemia). Mean blood pressure and
cardiac output may increase. Conversely, rapid lowering of the legs from the
lithotomy or Trendelenburg posi-tion acutely decreases venous return and can
result in hypotension. Vasodilation from either general or regional anesthesia
potentiates the hypotension in this situation, and for this reason, blood
pressure measurement should be taken immediately after the legs are lowered.
B. Choice of Anesthesia
General
anesthesia—Many patients
are appre-hensive about the procedure and prefer to be asleep. However, any
anesthetic technique suitable for out patients may be utilized. Because of the
short duration (15–20 min) and outpatient settingof
most cystoscopies, general anesthesia is often chosen, commonly employing a
laryngeal mask air-way. Oxygen saturation should be closely monitored when
obese or elderly patients, or those with mar-ginal pulmonary reserve, are
placed in the lithotomy or Trendelenburg position.
2.
Regional anesthesia—Both
epidural andspinal blockade provide satisfactory anesthesia for cystoscopy. However, when regional
anesthesia is chosen most anesthesiologists prefer spinal anesthesia because
onset of satisfactory sen-sory blockade may require 15–20 min for epidural
anesthesia compared with 5 min or less for spinal anesthesia. Some clinicians
believe that the sen-sory level following injection of a hyperbaric spi-nal
anesthetic solution should be well established (“fixed”) before the patient is
moved into the lithot-omy position; however, studies fail to demonstrate that
immediate elevation of the legs into lithotomy position following
administration of hyperbaric spinal anesthesia either increases the dermatomal
extent of anesthesia to a clinically significant de-gree or increases the
likelihood of severe hypoten-sion. A sensory level to T10 provides excellent
an-esthesia for essentially all cystoscopic procedures.
Related Topics