Chapter: Clinical Anesthesiology: Anesthetic Management: Obstetric Anesthesia
Anesthesia for Cesarean Section
Anesthesia for Cesarean Section
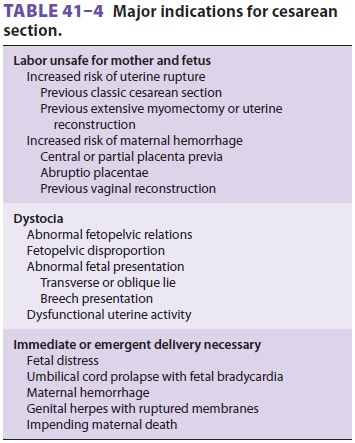
Common indications for cesarean section are
listed in Table 41–4. The choice of
anesthesia for cesarean section is determined by multiple factors, including
the indication for operative delivery, its urgency, patient and obstetrician
preferences, and the skills of the anesthetist. In a given country, cesarean
section rates may vary as much as two-fold between institutions. In some
countries, cesarean delivery is seen as preferable to labor and rates are much
greater than those in the United States (which generally vary between 15% and
35% from hospital to hospital). In the United States most elective cesarean
sections are performed under spinal anesthesia. Regional anesthesia has become
the preferred technique becausegeneral anesthesia has been associated with a
greater risk of maternal morbidity and mortality. Deaths associated with
general anesthesia are gen-erally related to airway problems, such as inability
to intubate, inability to ventilate, or aspiration pneumonitis, whereas deaths
associated with regional anesthesia are generally related to exces-sive
dermatomal spread of blockade or to local anesthetic toxicity.
Other advantages of regional anesthesia
include (1) less neonatal exposure to potentially depressant
drugs, (2) a decreased risk of maternal
pulmonary aspiration, (3) an awake mother at the birth of her child, and (4)
the option of using spinal opioids for postoperative pain relief. Continuous
epi-dural anesthesia allows better continuingcontrol over the sensory level
than “single-shot” techniques. Conversely, spinal anesthesia has a more rapid,
predictable onset; may produce a more dense (complete) block; and lacks the
potential for serious systemic drug toxicity because of the smaller dose of
local anesthetic employed. Regardless of the regional technique chosen, one
must be prepared to administer a general anesthetic at any time during the
procedure. Moreover, administration of a non-particulate antacid within 30 min
of surgery should be considered.
General anesthesia offers (1) a very rapid
and reliable onset, (2) control over the airway and venti-lation, (3) greater
comfort for parturients who have morbid fears of needles or surgery, and (4)
potentially less hypotension than regional anesthesia. General anesthesia also
facilitates management in the event of severe hemorrhagic complications such as
placentaaccreta. Its principal disadvantages are the risk of pulmonary
aspiration, the potential inability to intu-bate or ventilate the patient, and
drug-induced fetal depression. Present anesthetic techniques, however, limit
the dose of intravenous agents such that fetal depression is usually not
clinically significant with general anesthesia when delivery occurs within 10 min
of induction of anesthesia. Regardless of the type of anesthesia, neonates
delivered more than 3 min after uterine incision have lower Apgar scores and pH
values.
Related Topics