Chapter: Clinical Anesthesiology: Anesthetic Management: Ambulatory, Non operating Room, & Office-Based Anesthesia
Anesthesia: Specific Patient Conditions and Ambulatory Surgery
SPECIFIC PATIENT CONDITIONS AND AMBULATORY SURGERY
Obesity and Obstructive Sleep Apnea
Obesity is associated with many concomitant
dis-ease states, such as hypertension, diabetes, hyper-lidipemia, and
obstructive sleep apnea (OSA). The physiologic derangements that accompany
these conditions include changes in oxygen demand, car-bon dioxide production,
alveolar ventilation, and cardiac output. Patients with obesity and OSA are at
increased risk of postoperative respiratory compli-cations, such as prolonged
airway obstruction and apnea. Scores for predicting the probability of these
complications can aid in the preoperative assessment and referral to a hospital
setting (Tables 44–1 and 44–2). Although a sleep study is the standard way to
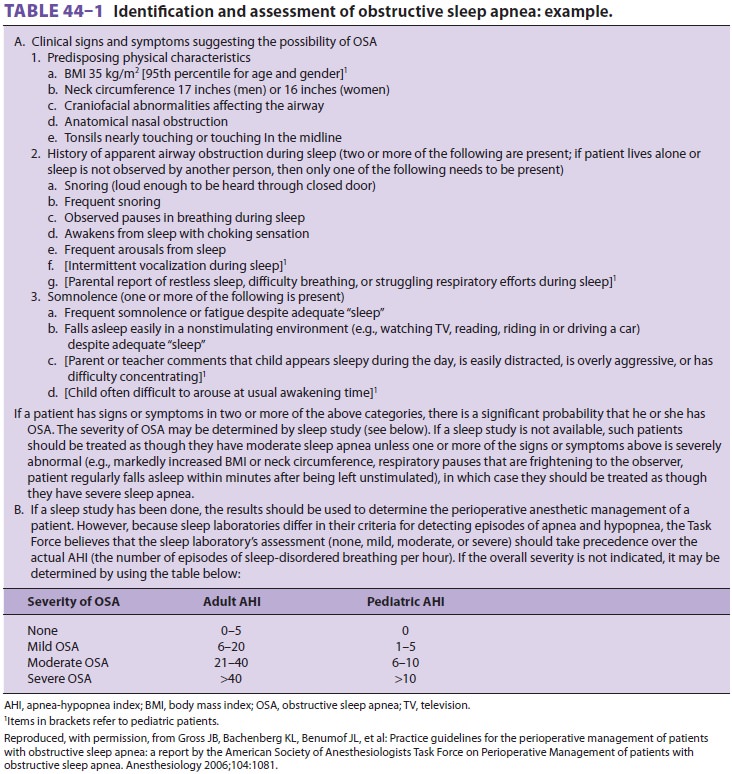
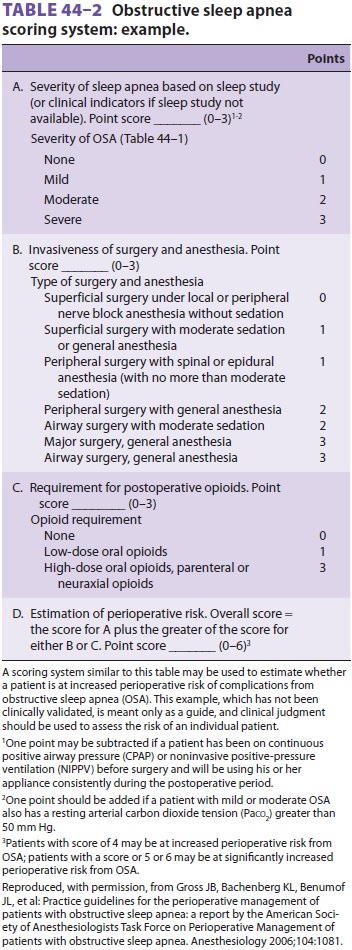
diagnose sleep apnea, many patients with OSA
have never been identified as having OSA. Consequently, an anesthesiologist may
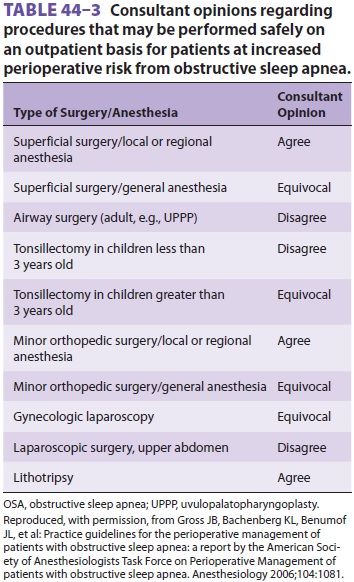
be the first physician to detect the presence or risk of sleep apnea. The ASA
has provided suggestions on the types of procedures and anesthetics that can
safely be used in ambula-tory patients with OSA (Table 44–3). In addition to the usual discharge criteria, the ASA also recom-mends
the following in patients with OSA:
·
Return of room air oxygen saturation
to baseline level
· No hypoxemic episodes or periods of airway obstruction when left alone
·
Monitoring for 3 hours longer prior
to discharge than patients without OSA
·
Monitoring for 7 hours following an
episode of airway obstruction or hypoxemia while breathing room air in an
unstimulating environment
According to the ASA Task Force on Obesity
and OSA, these OSA patients can be managed safely as outpatients; however, they
have an increased risk of postoperative complications requiring increased
monitoring, availability of radiologic/laboratory ser-vices, and availability
of continuous positive airway pressure and mechanical ventilation, thus making
an office-based setting potentially inadequate for man-aging complications that
may arise. Nonetheless, under certain conditions, anesthesia and surgery
can be performed in an ambulatory surgery center or hospital outpatient
facility.
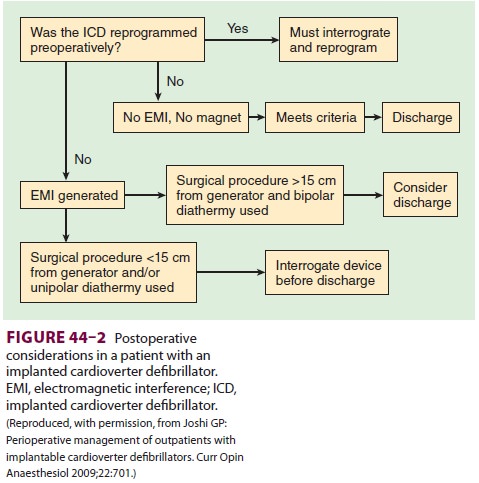
Cardiac Conditions
Increasingly, patients present to ambulatory
sur-gery with a variety of cardiac conditions treated both pharmacologically
and mechanically (eg, car-diac resynchronization therapy, implantable
cardio-verter-defibrillators [ICDs], stents). It is therefore likely that
anesthesia staff working in ambulatory settings will encounter increasing
numbers of such patients, who, despite a cardiac history, have stable cardiac
conditions. Patients previously treated with stents are likely to be on
antiplatelet regimens. As always, these agents should not be discontin-ued
unless a discussion has occurred between the patient, cardiologist, and surgeon
regarding both the necessity of surgery and the discontinuation of antiplatelet
therapy. Likewise, β-blockers should be
continued perioperatively. Angiotensin-converting enzyme inhibitors and
angiotensin receptor block-ers may contribute to transient hypotension with
anesthesia induction, but their continuation or dis-continuation
perioperatively seems to have minimal effects, as patients so treated likely
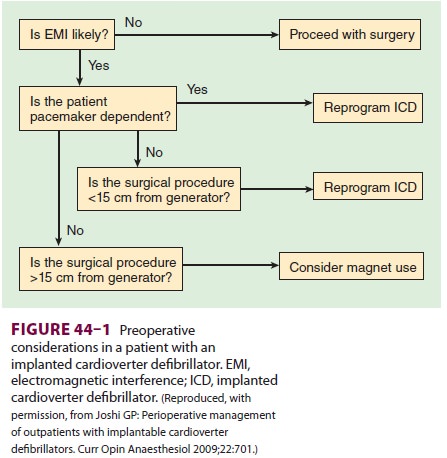
will need to have intraoperative hypotension corrected in either case. The ASA
guidelines recommend that patients pre-senting with a pacemaker or ICD should
not leave a monitored setting until the device is interrogated, if
electrocautery was employed; however, this ASA recommendation is controversial,
as some argue that if bipolar cautery is used at a distance of greater than 15
cm from the device, immediate interrogation of the device is not necessary
prior to discharge from a monitored setting. Likewise, if an ICD is present,
and there is anticipated electromagnetic interference the device’s
antitachycardia features should be inhib-ited perioperatively (see Figures
44–1 and 44–2).
Glucose Control
In a consensus statement on perioperative glucose control, the Society
for Ambulatory Anesthesia found insufficient evidence to make strong
recom-mendations about glucose management in ambu-latory patients, and thus
management suggestions parallel those of the inpatient population; however, the
panel recommends a target intraoperative blood glucose concentration of <180 mg/dL.
Malignant Hyperthermia
Patients with a history of malignant hyperthermia can be safely given
nontriggering anesthetics and discharged as ambulatory patients. Prophylactic
dantrolene should not be administered.
Related Topics