Chapter: The Massage Connection ANATOMY AND PHYSIOLOGY : Respiratory System
Anatomy of the Respiratory System
The Anatomy of the Respiratory
System
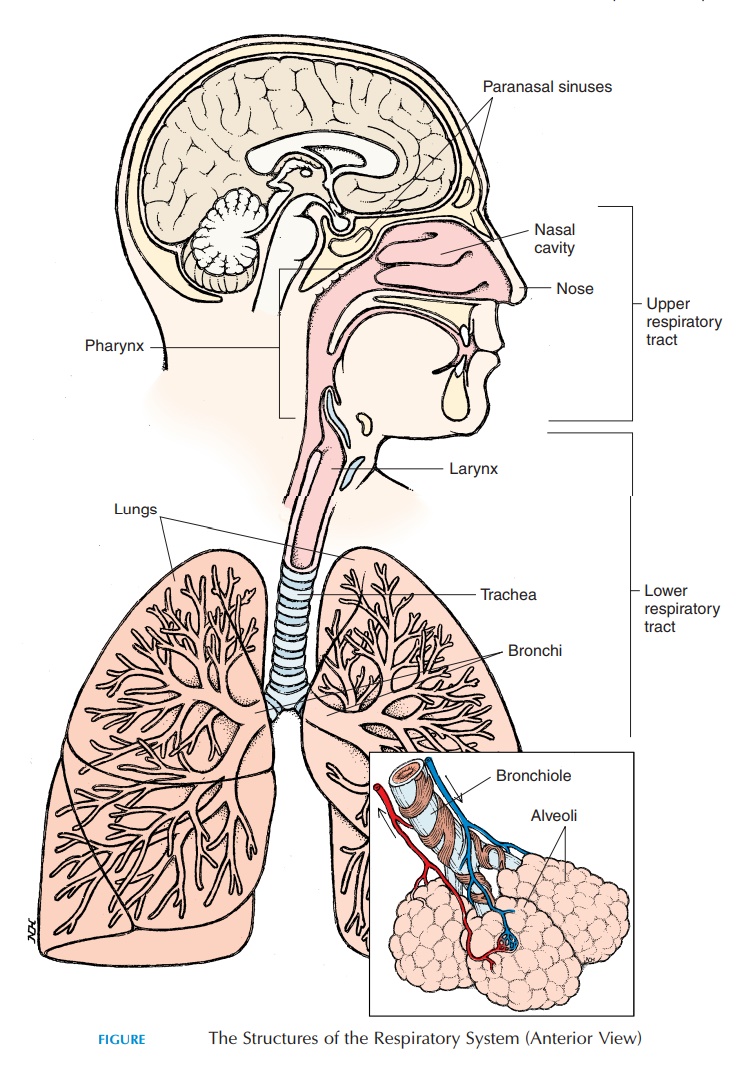
The respiratory system is made up of passages that conduct air from the environment into the body and respiratory surfaces that are involved in gas ex-change. The respiratory system is classically divided into the upper and lower respiratory tracts. The upper respiratory tract includes the nose, nasal cav-ity, paranasal sinus, and thepharynx (throat). Thelower respiratory tract (larynx and below) includes all structures below the pharynx and includes the larynx (voice box), trachea (wind pipe),bronchi, bronchioles, and the alveoli of the lungs (see Figure10.1). Functionally, the respiratory system can be classified as the conducting part and the respiratory part. The conducting part includes those structures that are only involved in conducting the air from the atmosphere to the lungs. All structures from the nose to the last part of the bronchioles belong to this cate-gory. The respiratory part includes the structures where gas exchange takes place and includes the last part of the bronchioles and distal structures.
UPPER RESPIRATORY TRACT
The Nose and Nasal Cavity
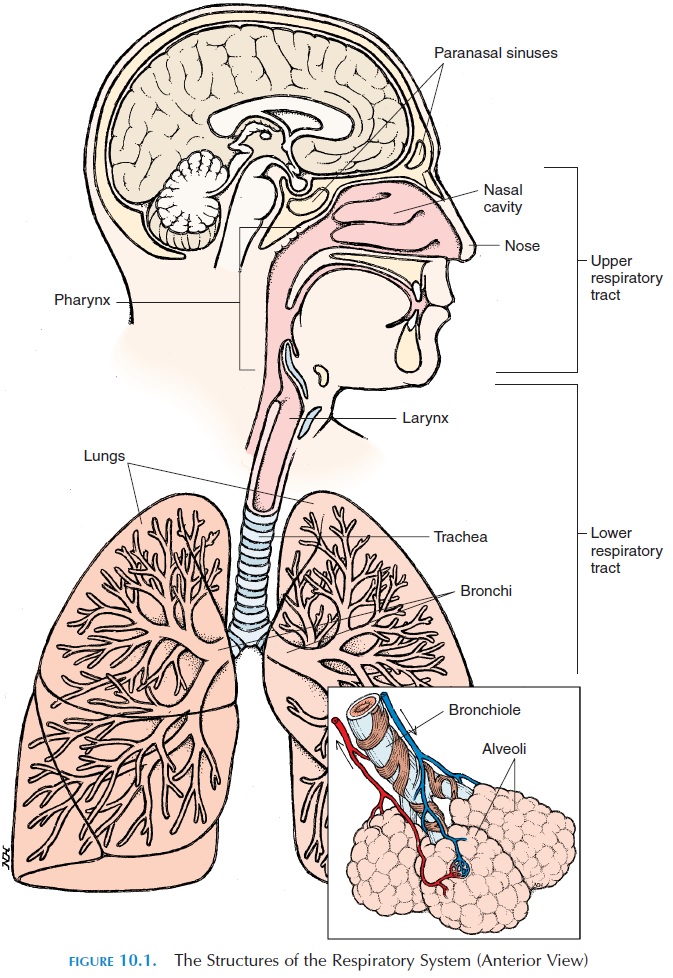
The air that reaches the lungs enters the body through the nose. The external part of the nose is made up of bone, hyaline cartilage, muscle, adipose tissue, and skin and is lined internally by mucous membrane. The superior part of the nose is bony; made up of the frontal, nasal, and maxillary bones. The inferior part is cartilaginous and more flexible. The openings on the inferior aspect of the nose are known as the nostrils, or external nares. The nostrils open internally into a wider area known as the nasal cavity (see Figure 10.2). The nasal cavity is divided into the right and the left regions by the nasal septum. The anterior and in-ferior portion of the nasal septum is made of hyaline cartilage (feel it); the superior part is made up of bone. Inferiorly, the nasal cavity is separated from the oral cavity by the maxillary and palatine bones; this is thehard palate, the hard portion of the roof of themouth. From the posterior part of the hard palate, a fleshy partition—the soft palate—separates the phar-ynx into thenasopharynx and oropharynx.
The first portion of the nasal cavity widens into the vestibule, which is the part seen when looking up thenostrils. This region is covered with coarse hair that extends across the nostrils and helps prevent larger particles, such as sand and sawdust, from entering the nasal cavity.
The nasal cavity is divided into smaller chambers by three, irregular, shelflike projections from the lat-eral wall of the nose known as the superior, middle, and inferior conchae. The air passes through the passages—the superior, middle, and inferior mea-tus—that are present between the conchae. The me-andering, turbulent pathway for air created by the conchae helps churn the air that has entered and en-ables large particles to stick to the mucus lining, slowing entry and providing sufficient time for the air to be altered to the body temperature and become saturated with water. In addition, the eddy produced carries air to the superior region of the nasal cavity where the smell receptors (olfactory receptors) are located. The posterior part of the nasal cavity opens into the pharynx through the internal nares.
Other than the external and internal nares, the nasal cavity has many other openings. The nasolacrimalduct—the tear duct that opens into the nose from theconjunctiva of the eye. This is the reason why the nose becomes “leaky” when a person cries. The tears that en-ter the nose keep the cavity moist. The openings of the paranasal sinus are located in the nose.
The Nasal Epithelium
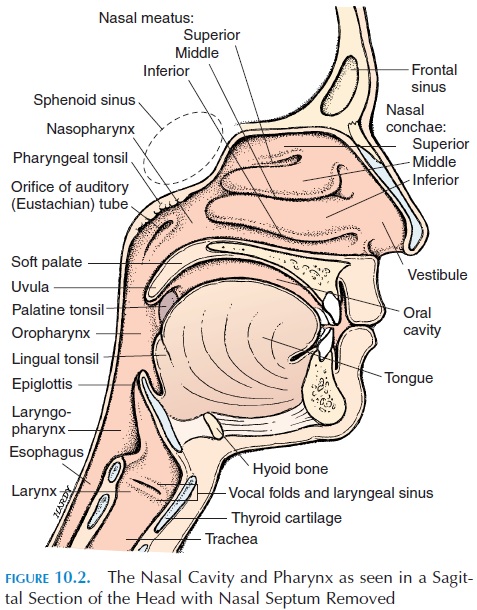
The nasal epithelium, or mucosa, is suited to clean the air that enters the nasal cavity and to bring it to body temperature and humidity. As mentioned, coarse hair prevents large particles from entering. The epithelium is a stratified squamous type that can withstand abrasion and friction. Then the epithelium changes to pseudostratified ciliated columnar ep-ithelium. The cilia, tiny hairlike projections on thecell membrane, move rhythmically in one direction.
Interspersed among the ciliated columnar cells are goblet cells, which secrete a sticky mucus (see Figure10.3). The cilia of the epithelium help move the mu-cus, together with any adhering dust and pathogens, toward the back of the nose. The movement of the cilia and mucus, similar to the movement of a con-veyor belt, is sometimes referred to as the mucous es-calator. From the back of the nose, the mucus enters the pharynx and is eventually swallowed.
The connective tissue lining the epithelium (lam-ina propria) contains many mucous glands, whichsecrete mucus into the nasal cavity, and a large net-work of blood vessels. These vessels help bring warm blood close to the surface. This mechanism helps warm and humidify the cool, dry air that enters. This process is important because the body can lose a lot of heat and moisture via the breathed air. Lower animals, such as dogs, use this mechanism for cooling the body by panting.
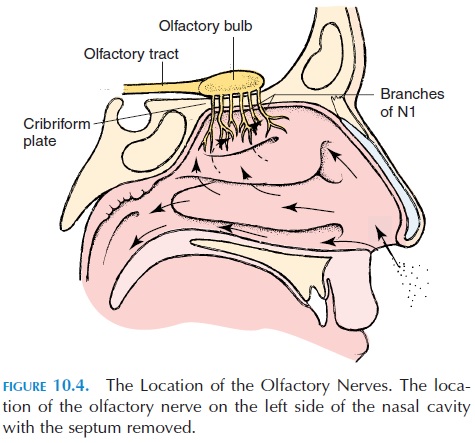
The Olfactory Mucosa
The superior part of the nasal cavity has specialized tissue that contains the nerve endings of the first cra-nial nerve—the olfactory nerve. These nerve endings, receptors for the sense of smell, are located along the superior nasal conchae, the superior portion of the nasal septum, and the inferior part of the cribriform plate (see Figure 10.4). The receptors are stimulated by chemicals in the air that dissolve in the mucous secretion. The olfactory nerves penetrate the tiny openings in the cribriform plate and carry the sense of smell to the brain. To get a better sense of a smell, we sniff forcefully to draw air in and reach the por-tion of the nasal cavity that houses the olfactory ep-ithelium .
Paranasal Sinus
The paranasal sinus (see Figure 10.5), or air cells of the nose, are cavities present in the lateral and supe-rior walls of the nasal cavity. The sphenoid sinus— located posteriorly and superiorly—are closely re-lated to the pituitary gland; therefore, the pituitary gland is often approached for surgery through the nasal cavity and the sphenoid sinus. The paired max-illary sinus are located in the maxillary bones. Themaxillary sinus have a greater tendency to become inflamed (sinusitis) because the sinus opening to the nasal cavity is located closer to the roof of the sinus (rather than the floor), making drainage more diffi-cult. There are many ethmoid sinus located in the ethmoid bone in the superior and posterior part of the nasal cavity. The frontal sinus are located deep to the medial part of the eyebrows. All of these sinus are air-filled cavities that communicate with the nasal cavity, and they are lined by the same epithelium as the rest of the nasal cavity.
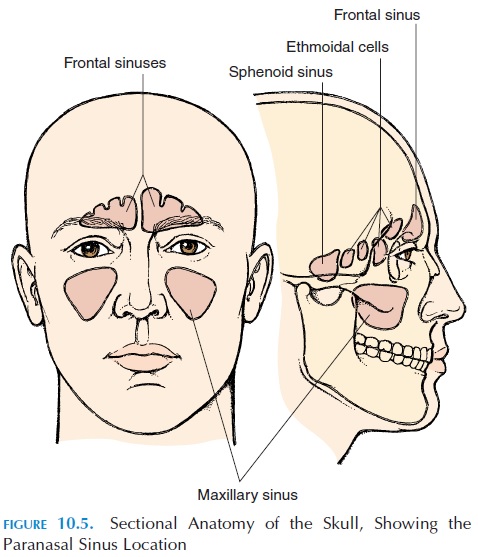
The sinus help humidify and heat the air that en-ters the body. In addition, they lighten the weight of the head. The resonance produced as a result of their presence gives the voice its specific characteristics.
The Pharynx
The region that extends between the posterior part of the nasal cavity—the internal nares and the larynx—is known as the pharynx (Figure 10.2). Both the respira-tory and digestive systems share part of this region. The superior wall of the pharynx is in close contact with the axial skeleton; the lateral walls are muscular. The pharynx is divided into three parts: the na-sopharynx, the oropharynx, and the laryngophar-ynx (Figures 10.1 and 10.2).
Nasopharynx
The nasopharynx region extends between the internal nares and the soft palate and lies superior to the oral cavity. Some lymphoid tissue—the pharyngeal tonsils or theadenoids—are located in the posterior wall.
The Eustachian tubes, or auditory tubes, which connect the middle ear to the pharynx, open into the nasopharynx. The opening opens and closes, equaliz-ing the air pressure in the middle ear to that of the at-mosphere. This is needed for proper conduction of sound.
Oropharynx
The oropharynx is the region of the pharynx that is common for the passage of food and air. This region lies between the soft palate and the base of tongue. The epithelium lining the oropharnyx changes from the delicate, pseudostratified ciliated columnar of the nasopharynx to the rugged, stratified squamous ep-ithelium because there is scope for abrasion and fric-tion from food. The posterior part of the tongue con-tains some lymphoid tissue—the lingual tonsils. The palatine tonsils are located to the side. Thus, thetonsils prevent passage of pathogens beyond this point.
Laryngopharynx, or Hypopharynx
The inferior most region of the pharynx is the laryn-gopharynx. The larynx is located anterior to the laryngopharynx.
LOWER RESPIRATORY TRACT
The Larynx
The larynx, or voice box (see Figure 10.6), is the re-gion that connects the pharynx to the trachea (wind-pipe). It can be felt just below the jaw in the upper, anterior part of the neck. The larynx is largely carti- lage, with ligaments and muscles attached. The epiglottis, thyroid cartilage, and cricoid cartilage are the larger cartilages. The epiglottis, located inter-nally close to the base of the tongue, is shaped like a shoehorn. With each swallow, it moves posteriorly to close the narrow opening of the larynx (the glottis) to prevent entry of food into the larynx.
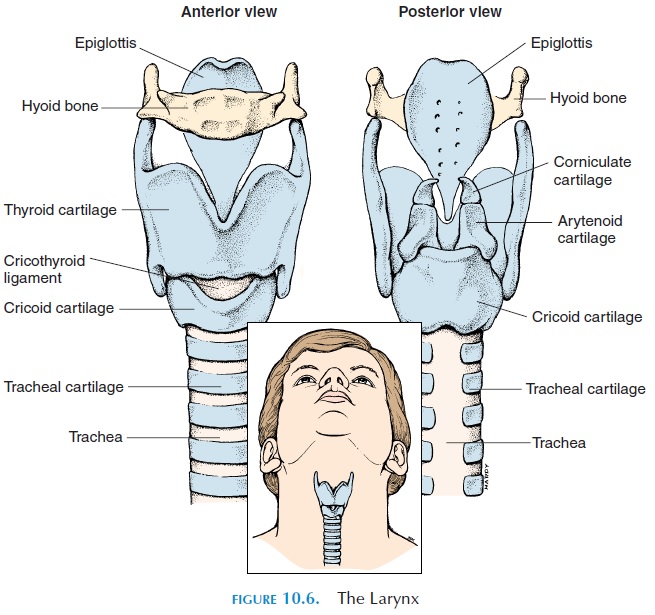
The thyroid cartilage is shaped like a shield and is commonly known as the Adam’s apple. It forms the anterior and lateral wall of the larynx. Superiorly, lig-aments attach the thyroid cartilage to the hyoid bone. Inferiorly, ligaments attach it to the cricoid cartilage. The cricoid cartilage is ring-shaped and is, in turn, inferiorly attached to the cartilage of the trachea (Figure 10.6).
Vocal Cords
Other smaller cartilages—arytenoids, cuneiform, and corniculate—elastic ligaments, and tiny muscles are located in the larynx. Two elastic ligaments, known as the true vocal cords, extend between the thyroid cartilage and arytenoid cartilage and go across the glottis. These ligaments are stretched and relaxed by laryngeal muscles that move the cartilage. The air that passes through the opening vibrates the vocal cords and produces sound. The size of the glottis and the length and tension of the vocal cords de-termine the pitch of the sound produced.
In males at puberty, the larynx enlarges in size and the vocal cords thicken and lengthen, making the voice deeper and lower pitched. Just superior to the true vocal codes are folds of mucosa known as the false vocalcords, or ventricular folds. The mucosa inferior tothe vocal cords is lined with pseudostratified ciliated columnar epithelium.
The sound production in the larynx is known as phonation. However, for words to be formed, thissound must be modified by articulation. Articulation requires voluntary muscle movement of the lips, cheeks, and tongue, etc. The pharynx, mouth, nasal cavity, and sinus act as resonating chambers.
Cough Reflex
The larynx contains sensitive nerves that trigger the cough reflex if food particles inadvertently enter this region. The cough reflex results in deep inspiration, followed by contraction of the expiratory muscles, with the glottis closed and the vocal cords tightened. This results in increased lung pressure. Suddenly, the glottis is opened, allowing a forceful blast of air to come through, dislodging the irritant from the laryn-geal region into the pharynx and beyond.
The Trachea
The trachea (Figures 10.1 and 10.7) is a tube about 11 cm (4.3 in) long and 2.5 cm (1 in) wide. It extends from the cricoid cartilage to the T5 vertebra, where it branches in two—the right and left primarybronchi. It is kept patent by 16–20 C-shaped carti-lage (the opening of the C faces posteriorly), attached to each other by ligaments. The posterior part of the trachea is closed off by a smooth muscle, the tra-chealis muscle. The cartilage prevents the tracheafrom collapsing every time there is a pressure change produced between the inside of the trachea and the atmosphere (in the neck region) as one breathes. The softer, posterior aspect of the trachea allows for ex-pansion of the esophagus as food passes.
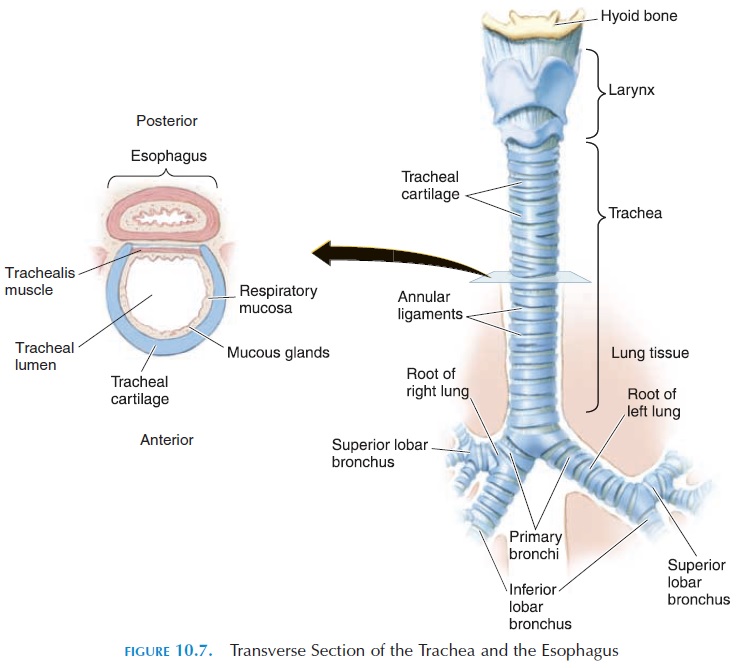
The Bronchi and Bronchioles
The trachea branches into the right and left primarybronchi at the level of the second costal cartilage atthe sternal angle (superior border of the fifth thoracic vertebra) in the mediastinum. Both bronchus have cartilage similar to the trachea, with the right bronchus wider and more in line with the trachea. Therefore, foreign particles that enter the trachea (a rare occurrence) tend to lodge in this bronchus. The bronchi enter the lungs at the hilus, the medial re-gion of the lung, through which blood vessels, nerves, lymphatics, and bronchi enter.
The primary bronchi divide repeatedly to form smaller bronchi and bronchioles. The bronchi located outside the lungs are known as extrapulmonarybronchi and the remainder, intrapulmonary bronchi.
The primary bronchi divide into three on the right and two on the left known as lobar, or secondary bronchi.
Each bronchus moves air in and out of the respective lobes of the lungs (see below). The lobar bronchi be-come smaller and branch again to form the tertiary, orsegmental bronchi. The tertiary bronchi branch fur-ther to form tiny, terminal bronchioles, which are about 0.3–0.5 mm (0.01–0.02 in) wide.
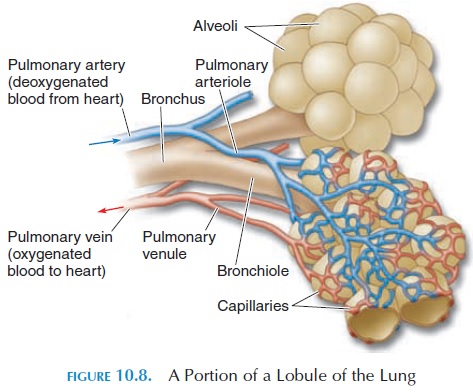
The lung tissue supplied by each tertiary bronchi is called a bronchopulmonary segment. There are ten bronchopulmonary segments in each lung, each made of many lobules. Each lobule (see Figure 10.8) is wrapped in elastic connective tissue and has an ar-teriole, venule, lymphatic vessel, and a branch from the terminal bronchiole. If there are tumors or ab-scesses in any bronchopulmonary segment, the seg-ment can be surgically removed without affecting the surrounding lung tissue. Knowledge of the direction of bronchi supplying the segments helps therapists facilitate drainage of secretions from specific seg-ments by changing the posture of the patient.
All structures from the nasal cavity to the terminal bronchiole serve only as conducting passages for the air that enters. Exchange of gases between the air and the blood only takes place in the region of the respiratory bronchioles and beyond.
Bronchial Smooth Muscle and Its Control
Bronchi walls lose cartilage as they branch and be-come smaller. Instead, the walls have more smooth muscle. Contraction and relaxation of these smooth muscles alter the caliber of the bronchi and bronchi-oles regulating the volume of air entering different re-gions of the lungs. The smooth muscles of the bronchi and bronchioles are innervated by the autonomic sys-tem. The sympathetic nerves relax the smooth mus-cles and increase the caliber of the passages, making it easier for air to enter the lungs; the parasympa-thetic nerves have the opposite action. In addition to nerves, chemicals such as leukotrienes and substance P, secreted locally by white blood cells and other cells, have an effect on bronchial smooth muscles. This is why asthma tends to worsen during, or soon after, res-piratory infections in which white blood cell activity is increased. Also, allergen exposure and resultant in-flammation can trigger an asthmatic attack.
The Alveoli
The respiratory bronchioles are connected to larger spaces, called alveolar ducts, into which open smaller chambers known as the alveoli (Figure 10.8). The alveoli (singular, alveolus) are lined by a single layer of squamous cells. The alveoli walls contain elastic fibers that help reduce the volume of the alveoli when air is breathed out. The alveoli give the lungs a spongy ap-pearance. The alveoli increase the surface area for ex-change of gases; each lung contains about 150 million alveoli. The total surface area made available for gas exchange by the alveoli is approximately 150 m2 (179 yd2). The alveoli are surrounded by an extensive net-work of capillaries. Thus, the air that enters the alveoli is separated from the blood by only the thin, single layer of endothelium of the capillaries, a basement membrane, and the thin wall of the alveoli—a distance of about 0.1µm. These layers that separate air from blood are known as the respiratory membrane.
Alveoli Defense and Lubrication
Many macrophages patrol the alveoli and eliminate pathogens that have escaped other defense mecha-nisms of the respiratory system. The thin, moist lining of the spherical alveoli tends to collapse and stick together because of surface ten-sion. (Surface tension is the force produced by the at-traction of water molecules to each other. When wa-ter surrounds gas, the attraction between the water molecules rather than between air and water, pro-duces a force that is directed inward. It is surface ten-sion that causes a drop of water to attain a spherical shape.) Specialized cells, known as type II cells, sep-tal cells, or surfactant cells, produce an oily secre-tion (surfactant), which lubricates and reduces the surface tension of the liquid coating the alveoli. Sur-factant is a detergentlike mixture of phospholipids and lipoprotein. If not present in sufficient amounts, it will be difficult for air to enter the alveoli, similar to the difficulty faced when two, wet, glass surfaces, placed one over the other, are pried apart. In the ab-sence of surfactant, the alveoli tend to collapse dur-ing expiration.
THE PULMONARY CIRCULATION
The blood reaching the alveoli is that of the pulmonary circulation . Blood that has circulated through the body, with most of the oxygen removed, enters the right ventricle via the superior and inferior vena cava. Contraction of the right ventricle pumps this blood into the pulmonary trunk. The pulmonary trunk divides into right and left branches, which take the blood to the right and left lungs, respectively. As in all organs, the arteries divide to form arterioles and capillaries. It is this network of capillaries that sur-round the alveoli and participate in gas exchange. The capillaries join and rejoin to form venules and veins. Ultimately, four pulmonary veins transport the oxygenated blood into the leftatrium, where they enter the left ventricle and then are pumped into the aorta and distributed to the rest of the body. Bronchial arteries—branches from the aorta—bring oxygenated blood to the bronchi and other lung tissue. Most blood from the bronchial ar-teries returns to the heart via the pulmonary veins. Some reach the heart through veins that ultimately reach the heart via the superior vena cava.
The blood vessels in the lungs, unlike those in other tissue, constrict when there is less oxygen in the surrounding region. This is advantageous be-cause it helps direct blood to better-ventilated parts of the lung.
THE LUNGS
The paired lungs are organs comprised of bronchi, bronchioles, alveoli, connective tissue, blood vessels, lymphatics, and nerves (see Figure 10.9). The right and left lungs are situated on either side of the medi-astinum (the part of the thoracic cavity that lies be-tween the lungs). The lung is somewhat conical, with the apex projecting just above the first rib. The base of the lung is related to the superior surface of the di-aphragm, which separates the thorax from the ab-domen. The lungs take the same contour as the inner wall of the thorax, and the lung surface in contact with the thoracic wall is known as the costal sur-face. Medially, the mediastinal surface of the lung isin contact with the structures of the mediastinum.
The lungs are separated into lobes by deep fissures. The right lung has three lobes (the superior, middle, and inferior); the left lung has only two lobes (the su-perior andinferior). A deep, oblique fissure sepa-rates the superior and the inferior lobe. In the right, a horizontal fissure separates the superior and themiddle lobes. The right lung appears larger than the left lung; in the left, a lot of space is taken by the heart and great blood vessels. The right lung is shorter, how-ever, because the diaphragm is higher in the right as a result of the presence of the liver inferiorly.
THE PLEURA
The pleura membrane surrounds the lungs. Similar to the pericardial membrane and pericardial cavity, the pleura is a double membrane with a cavity in be-tween (Figure 10.9). The layer in close contact with the lungs is the visceral pleura.
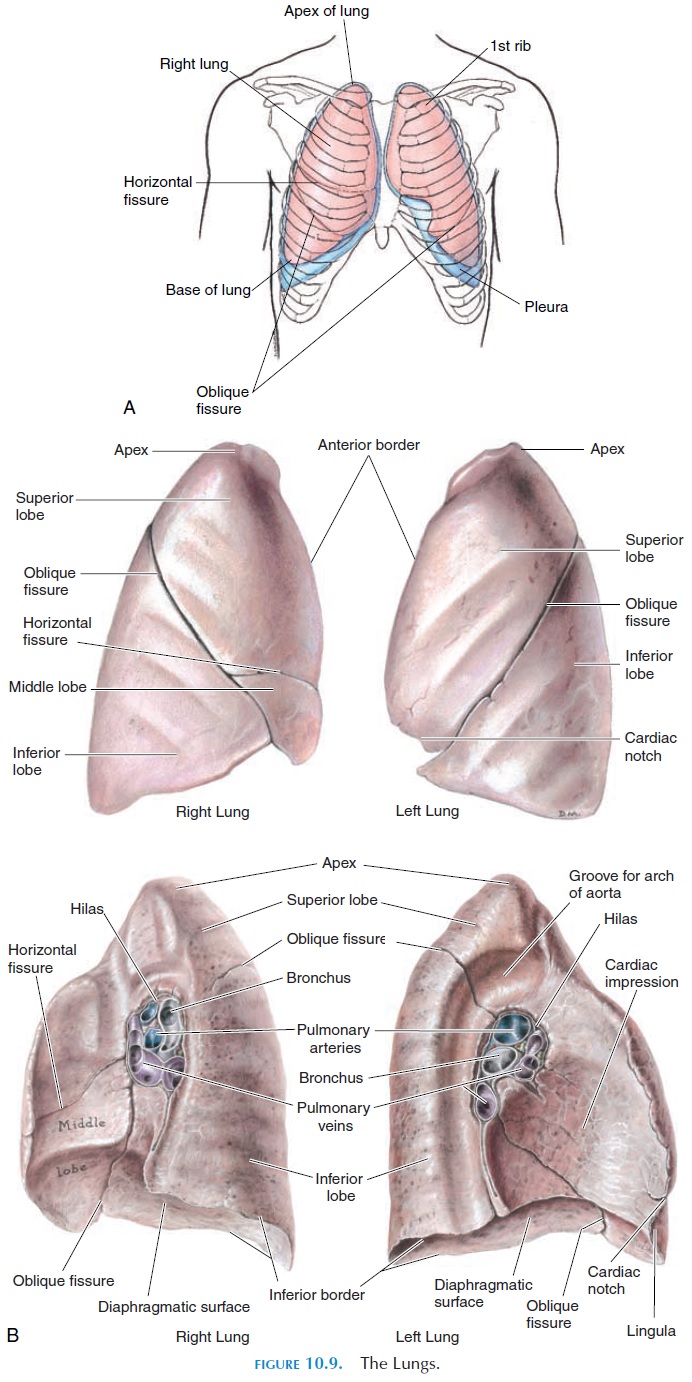
The other layer lines the thoracic cavity, diaphragm, and the mediastinum (other than the hilus) and is known as the parietalpleura. A good analogy of the pleural cavity anatomyis to think of the lung as a fist being pushed into a balloon partly filled with air. The layer of the balloon close to the fist would be the equivalent to the visceral pleura; the other layer, the parietal pleura. The space between the layers, the pleural cavity, is filled with some fluid (pleural fluid) rather than air as in the balloon. The pleural fluid provides lubrication and minimizes friction when the lungs move during breathing.
Related Topics