Chapter: Medical Physiology: Kidney Diseases and Diuretics
Acute Renal Failure
Acute Renal Failure
The causes of acute renal failure can be divided into three main categories:
1. Acute renal failure resulting from decreased blood supply to the kidneys; this condition is often referred to as prerenal acute renal failure to reflect the fact that the abnormality occurs in a system beforethe kidneys. This can be a consequence of heart failure with reduced cardiac output and low blood pressure or conditions associated with diminished blood volume and low blood pressure, such as severe hemorrhage.
2. Intrarenal acute renal failure resulting fromabnormalities within the kidney itself, including those that affect the blood vessels, glomeruli, or tubules.
3. Postrenal acute renal failure, resulting fromobstruction of the urinary collecting system anywhere from the calyces to the outflow from the bladder. The most common causes of obstruction of the urinary tract outside the kidney are kidney stones, caused by precipitation of calcium, urate, or cystine.
Prerenal Acute Renal Failure Caused by Decreased Blood Flow to the Kidney
The kidneys normally receive an abundant blood supply of about 1100 ml/min, or about 20 to 25 per cent of the cardiac output.The main purpose of this high blood flow to the kidneys is to provide enough plasma for the high rates of glomerular filtration needed for effective regu-lation of body fluid volumes and solute concentrations. Therefore, decreased renal blood flow is usually accom-panied by decreased GFR and decreased urine output of water and solutes. Consequently, conditions that acutely diminish blood flow to the kidneys usually cause oliguria, which refers to diminished urine output belowthe level of intake of water and solutes.This causes accu-mulation of water and solutes in the body fluids. If renal blood flow is markedly reduced, total cessation of urine output can occur, a condition referred to asanuria.
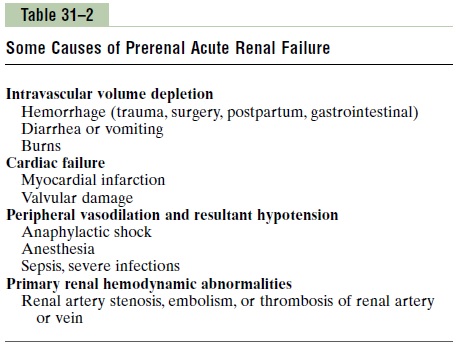
As long as renal blood flow does not fall below about 20 to 25 per cent of normal, acute renal failure can usually be reversed if the cause of the ischemia is cor-rected before damage to the renal cells has occurred. Unlike some tissues, the kidney can endure a relatively large reduction in blood flow before actual damage to the renal cells occurs. The reason for this is that as renal blood flow is reduced, the GFR and the amount of sodium chloride filtered by the glomeruli (as well as the filtration rate of water and other electrolytes) are reduced. This decreases the amount of sodium chloride that must be reabsorbed by the tubules, which uses most of the energy and oxygen consumed by the normal kidney. Therefore, as renal blood flow and GFR fall, the requirement for renal oxygen consumption is also reduced. As the GFR approaches zero, oxygen con-sumption of the kidney approaches the rate that is required to keep the renal tubular cells alive even when they are not reabsorbing sodium. When blood flow is reduced below this basal requirement, which is usually less than 20 to 25 per cent of the normal renal blood flow, the renal cells start to become hypoxic, and further decreases in renal blood flow, if prolonged, will cause damage or even death of the renal cells, especially the tubular epithelial cells. If the cause of prerenal acute renal failure is not corrected and ischemia of the kidney persists longer than a few hours, this type of renal failure can evolve into intrarenal acute renal failure, as dis-cussed later. Acute reduction of renal blood flow is a common cause of acute renal failure in hospitalized patients. Table 31–2 shows some of the common causes of decreased renal blood flow and prerenal acute renal failure.
Intrarenal Acute Renal Failure Caused by Abnormalities Within the Kidney
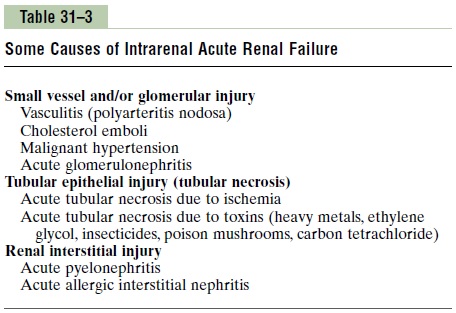
Abnormalities that originate within the kidney and that abruptly diminish urine output fall into the general cat-egory of intrarenal acute renal failure. This category of acute renal failure can be further divided into (1) conditions that injure the glomerular capillaries or other small renal vessels, (2) conditions that damage the renal tubular epithelium, and (3) conditions that cause damage to the renal interstitium. This type of classifica-tion refers to the primary site of injury, but because the renal vasculature and tubular system are functionally interdependent, damage to the renal blood vessels can lead to tubular damage, and primary tubular damage can lead to damage of the renal blood vessels. Causes of intrarenal acute renal failure are listed in Table 31–3.
Acute Renal Failure Caused by Glomerulonephritis. Acuteglomerulonephritis is a type of intrarenal acute renal failure usually caused by an abnormal immune reaction that damages the glomeruli. In about 95 per cent of the patients with this disease, damage to the glomeruli occurs 1 to 3 weeks after an infection elsewhere in the body, usually caused by certain types of group A beta streptococci. The infection may have been a streptococ-cal sore throat, streptococcal tonsillitis, or even strepto-coccal infection of the skin. It is not the infection itself that damages the kidneys. Instead, over a few weeks, as antibodies develop against the streptococcal antigen, the antibodies and antigen react with each other to form an insoluble immune complex that becomes entrapped in the glomeruli, especially in the basement membrane portion of the glomeruli.
Once the immune complex has deposited in the glomeruli, many of the cells of the glomeruli begin to proliferate, but mainly the mesangial cells that lie between the endothelium and the epithelium. In addi-tion, large numbers of white blood cells become entrapped in the glomeruli. Many of the glomeruli become blocked by this inflammatory reaction, and those that are not blocked usually become excessively permeable, allowing both protein and red blood cells to leak from the blood of the glomerular capillaries into the glomerular filtrate. In severe cases, either total or almost complete renal shutdown occurs.
The acute inflammation of the glomeruli usually sub-sides in about 2 weeks, and in most patients, the kidneys return to almost normal function within the next few weeks to few months. Sometimes, however, many of the glomeruli are destroyed beyond repair, and in a small percentage of patients, progressive renal deterioration continues indefinitely, leading to chronic renal failure.
Tubular Necrosis as a Cause of Acute Renal Failure. Anothercause of intrarenal acute renal failure is tubular necro-sis, which means destruction of epithelial cells in thetubules. Some common causes of tubular necrosis are (1) severe ischemia and inadequate supply of oxygen and nutrients to the tubular epithelial cells and (2) poisons, toxins, or medications that destroy the tubular epithelial cells.
Acute Tubular Necrosis Caused by Severe Renal Ischemia. Severe ischemia of the kidney can result fromcirculatory shock or any other disturbance that severely impairs the blood supply to the kidney. If the ischemia is severe enough to seriously impair the delivery of nutrients and oxygen to the renal tubular epithelial cells, and if the insult is prolonged, damage or eventual destruction of the epithelial cells can occur. When this happens, tubular cells “slough off” and plug many of the nephrons, so that there is no urine output from the blocked nephrons; the affected nephrons often fail to excrete urine even when renal blood flow is restored to normal, as long as the tubules remain plugged. The most common causes of ischemic damage to the tubular epithelium are the prerenal causes of acute renal failure associated with circulatory shock.
Acute Tubular Necrosis Caused by Toxins or Medications.There is a long list of renal poisons and medications that can damage the tubular epithelium and cause acute renal failure. Some of these are carbon tetrachloride, heavymetals (such as mercury and lead), ethylene glycol (whichis a major component in antifreeze), various insecticides, various medications (such as tetracyclines) used as antibiotics, and cis-platinum, which is used in treating certain cancers. Each of these substances has a specific toxic action on the renal tubular epithelial cells, causing death of many of them. As a result, the epithelial cells slough away from the basement membrane and plug the tubules. In some instances, the basement membrane also is destroyed. If the basement membrane remains intact, new tubular epithelial cells can grow along the surface of the membrane, so that the tubule repairs itself within 10 to 20 days.
Postrenal Acute Renal Failure Caused by Abnormalities of the Lower Urinary Tract
Multiple abnormalities in the lower urinary tract can block or partially block urine flow and therefore lead to acute renal failure even when the kidneys’ blood supply and other functions are initially normal. If the urine output of only one kidney is diminished, no major change in body fluid composition will occur because the contralateral kidney can increase its urine output suffi-ciently to maintain relatively normal levels of extracel-lular electrolytes and solutes as well as normal extracellular fluid volume. With this type of renal failure, normal kidney function can be restored if the basic cause of the problem is corrected within a few hours. But chronic obstruction of the urinary tract, lasting for several days or weeks, can lead to irreversible kidney damage. Some of the causes of postrenal acute failure include (1) bilateral obstruction of the ureters or renal pelvises caused by large stones or blood clots, (2) bladder obstruction, and (3) obstruction of the urethra.
Physiologic Effects of Acute Renal Failure
A major physiologic effect of acute renal failure is retention in the blood and extracellular fluid of water, waste products of metabolism, and electrolytes. This can lead to water and salt overload, which in turn can lead to edema and hypertension. Excessive retention of potassium, however, is often a more serious threat to patients with acute renal failure, because increases in plasma potassium concentration (hyperkalemia) to more than about 8 mEq/L (only twice normal) can be fatal. Because the kidneys are also unable to excrete sufficient hydrogen ions, patients with acute renal failure develop metabolic acidosis, which in itself can be lethal or can aggravate the hyperkalemia.
In the most severe cases of acute renal failure, com-plete anuria occurs. The patient will die in 8 to 14 days unless kidney function is restored or unless an artificial kidney is used to rid the body of the excessive retained water, electrolytes, and waste products of metabolism. Other effects of diminished urine output, as well as treatment with an artificial kidney, are dis-cussed in the next section in relation to chronic renal failure.
Related Topics