Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Biliary Disorders
Acute Pancreatitis - Disorders of the Pancreas
ACUTE
PANCREATITIS
Acute
pancreatitis ranges from a mild, self-limiting disorder to a severe, rapidly
fatal disease that does not respond to any treat-ment. Mild acute pancreatitis
is characterized by edema and in-flammation confined to the pancreas. Minimal
organ dysfunction is present, and return to normal usually occurs within 6
months. Although this is considered the milder form of pancreatitis, the
patient is acutely ill and at risk for hypovolemic shock, fluid and electrolyte
disturbances, and sepsis. A more widespread and com-plete enzymatic digestion
of the gland characterizes severe acute pancreatitis. The tissue becomes
necrotic, and the damage ex-tends into the retroperitoneal tissues. Local
complications consist of pancreatic cysts or abscesses and acute fluid
collections in or near the pancreas. Systemic complications, such as acute
respira-tory distress syndrome, shock, disseminated intravascular
coagu-lopathy, and pleural effusion, can increase the mortality rate to 50% or
higher (Aronson, 1999).
Gerontologic Considerations
Acute
pancreatitis affects people of all ages, but the mortality rate associated with
acute pancreatitis increases with advancing age. In addition, the pattern of
complications changes with age. Younger patients tend to develop local
complications; the incidence of multiple organ failure increases with age,
possibly as a result of progressive decreases in physiologic function of major
organs with increasing age. Close monitoring of major organ function (ie,
lungs, kidneys) is essential, and aggressive treatment is neces-sary to reduce
mortality from acute pancreatitis in the elderly.
Pathophysiology
Self-digestion
of the pancreas by its own proteolytic enzymes, principally trypsin, causes
acute pancreatitis. Eighty percent of patients with acute pancreatitis have
biliary tract disease; how-ever, only 5% of patients with gallstones develop
pancreatitis. Gallstones enter the common bile duct and lodge at the ampulla of
Vater, obstructing the flow of pancreatic juice or causing a re-flux of bile
from the common bile duct into the pancreatic duct, thus activating the
powerful enzymes within the pancreas. Nor-mally, these remain in an inactive
form until the pancreatic se-cretions reach the lumen of the duodenum.
Activation of the enzymes can lead to vasodilation, increased vascular
permeabil-ity, necrosis, erosion, and hemorrhage (Quillen, 2001).
Long-term
use of alcohol is commonly associated with acute episodes of pancreatitis, but
the patient usually has had un-diagnosed chronic pancreatitis before the first
episode of acute pancreatitis occurs. Other less common causes of pancreatitis
in-clude bacterial or viral infection, with pancreatitis a complication of
mumps virus. Spasm and edema of the ampulla of Vater, re-sulting from
duodenitis, can probably produce pancreatitis. Blunt abdominal trauma, peptic
ulcer disease, ischemic vascular disease, hyperlipidemia, hypercalcemia, and
the use of corticosteroids, thi-azide diuretics, and oral contraceptives also
have been associated with an increased incidence of pancreatitis. Acute
pancreatitis may follow surgery on or near the pancreas or after
instrumentation of the pancreatic duct. Acute idiopathic pancreatitis accounts
for up to 20% of the cases of acute pancreatitis (Hale, Moseley & Warner,
2000). In addition, there is a small incidence of hereditary pancreatitis.
The
mortality rate of patients with acute pancreatitis is high (10%) because of
shock, anoxia, hypotension, or fluid and elec-trolyte imbalances. Attacks of
acute pancreatitis may result in complete recovery, may recur without permanent
damage, or may progress to chronic pancreatitis. The patient admitted to the
hospital with a diagnosis of pancreatitis is acutely ill and needs expert
nursing and medical care.
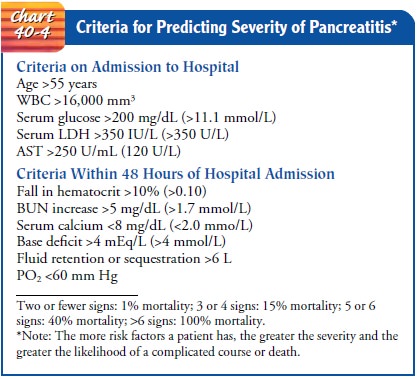
Severity
and mortality predictions of acute alcoholic pancre-atitis are generally
assessed using Ranson’s criteria (Tierney,McPhee& Papadakis, 2001). The
Acute Physiology and Chronic Health Evaluation (APACHE) grading system may also
be used. Predictors of the severity of pancreatitis and its prognosis are listed
in Chart 40-4.
Clinical Manifestations
Severe
abdominal pain is the major symptom of pancreatitis that causes the patient to
seek medical care. Abdominal pain and ten-derness and back pain result from
irritation and edema of the in-flamed pancreas that stimulate the nerve
endings. Increased tension on the pancreatic capsule and obstruction of the
pan-creatic ducts also contribute to the pain. Typically, the pain oc-curs in
the midepigastrium. Pain is frequently acute in onset, occurring 24 to 48 hours
after a very heavy meal or alcohol in-gestion, and it may be diffuse and
difficult to localize. It is gen-erally more severe after meals and is
unrelieved by antacids. Pain may be accompanied by abdominal distention; a
poorly defined, palpable abdominal mass; and decreased peristalsis. Pain caused
by pancreatitis is accompanied frequently by vomiting that does not relieve the
pain or nausea.
The
patient appears acutely ill. Abdominal guarding is pres-ent. A rigid or
board-like abdomen may develop and is generally an ominous sign; the abdomen
may remain soft in the absence of peritonitis. Ecchymosis (bruising) in the
flank or around the um-bilicus may indicate severe pancreatitis. Nausea and
vomiting are common in acute pancreatitis. The emesis is usually gastric in
ori-gin but may also be bile-stained. Fever, jaundice, mental confu-sion, and
agitation also may occur.
Hypotension
is typical and reflects hypovolemia and shock caused by the loss of large
amounts of protein-rich fluid into the tissues and peritoneal cavity. The
patient may develop tachycar-dia, cyanosis, and cold, clammy skin in addition
to hypotension. Acute renal failure is common.
Respiratory distress and hypoxia are common, and the patient may develop diffuse pulmonary infiltrates, dyspnea, tachypnea, and abnormal blood gas values. Myocardial depression, hypocal-cemia, hyperglycemia, and disseminated intravascular coagu-lopathy (DIC) may also occur with acute pancreatitis.
Assessment and Diagnostic Findings
The
diagnosis of acute pancreatitis is based on a history of ab-dominal pain, the
presence of known risk factors, physical exam-ination findings, and diagnostic
findings. Serum amylase and lipase levels are used in making the diagnosis of
acute pancreatitis. In 90% of the cases, serum amylase and lipase levels
usually rise in excess of three times their normal upper limit within 24 hours
(Tierney, McPhee & Papadakis, 2001). Serum amylase usually returns to
normal within 48 to 72 hours. Serum lipase levels may remain elevated for 7 to
14 days (Braunwald et al., 2001). Uri-nary amylase levels also become elevated
and remain elevated longer than serum amylase levels. The white blood cell
count is usually elevated; hypocalcemia is present in many patients and correlates
well with the severity of pancreatitis. Transient hyper-glycemia and glucosuria
and elevated serum bilirubin levels occur in some patients with acute
pancreatitis.
X-ray
studies of the abdomen and chest may be obtained to differentiate pancreatitis
from other disorders that may cause sim-ilar symptoms and to detect pleural
effusions. Ultrasound and contrast-enhanced computed tomography scans are used
to iden-tify an increase in the diameter of the pancreas and to detect
pan-creatic cysts, abscesses, or pseudocysts.
Hematocrit
and hemoglobin levels are used to monitor the pa-tient for bleeding. Peritoneal
fluid, obtained through paracente-sis or peritoneal lavage, may contain
increased levels of pancreatic enzymes. The stools of patients with pancreatic
disease are often bulky, pale, and foul-smelling. Fat content of stools varies
between 50% and 90% in pancreatic disease; normally, the fat content is 20%.
ERCP is rarely used in the diagnostic evaluation of acute pancreatitis because
the patient is acutely ill; however, it may be valuable in the treatment of
gallstone pancreatitis.
Medical Management
Management
of the patient with acute pancreatitis is directed to-ward relieving symptoms
and preventing or treating complica-tions. All oral intake is withheld to
inhibit pancreatic stimulation and secretion of pancreatic enzymes. Parenteral
nutrition is usu-ally an important part of therapy, particularly in debilitated
pa-tients, because of the extreme metabolic stress associated with acute
pancreatitis (Dejong, Greve & Soeters, 2001). Nasogastric suction may be
used to relieve nausea and vomiting, to decrease painful abdominal distention
and paralytic ileus, and to remove hydrochloric acid so that it does not enter
the duodenum and stimulate the pancreas. Histamine-2 (H2) antagonists (eg,
ci-metidine [Tagamet] and ranitidine [Zantac]) may be prescribed to decrease
pancreatic activity by inhibiting HCl secretion.
PAIN MANAGEMENT
Adequate
pain medication is essential during the course of acute pancreatitis to provide
sufficient pain relief and minimize rest-lessness, which may stimulate
pancreatic secretion further. Mor-phine and morphine derivatives are often
avoided because it has been thought that they cause spasm of the sphincter of
Oddi; meperidine (Demerol) is often prescribed because it is less likely to
cause spasm of the sphincter (Porth, 2002). Antiemetic agents may be prescribed
to prevent vomiting.
INTENSIVE CARE
Correction
of fluid and blood loss and low albumin levels is nec-essary to maintain fluid
volume and prevent renal failure. The pa-tient is usually acutely ill and is
monitored in the intensive care unit, where hemodynamic monitoring and arterial
blood gas monitoring are initiated. Antibiotic agents may be prescribed if
infection is present; insulin may be required if significant hyper-glycemia
occurs.
RESPIRATORY CARE
Aggressive
respiratory care is indicated because of the high risk for elevation of the
diaphragm, pulmonary infiltrates and effusion, and atelectasis. Hypoxemia
occurs in a significant number of pa-tients with acute pancreatitis even with
normal x-ray findings. Respiratory care may range from close monitoring of
arterial blood gases to use of humidified oxygen to intubation and me-chanical
ventilation.
BILIARY DRAINAGE
Placement
of biliary drains (for external drainage) and stents (in-dwelling tubes) in the
pancreatic duct through endoscopy has been performed to reestablish drainage of
the pancreas. This has resulted in decreased pain and increased weight gain.
SURGICAL INTERVENTION
Although
often risky because the acutely ill patient is a poor surgical risk, surgery
may be performed to assist in the diagnosis of pancreatitis (diagnostic
laparotomy), to establish pancreatic drainage, or to resect or débride a
necrotic pancreas. The patient who undergoes pancreatic surgery may have
multiple drains in place postoperatively as well as a surgical incision that is
left open for irrigation and repacking every 2 to 3 days to remove necrotic
debris (Fig. 40-6).

POSTACUTE MANAGEMENT
Antacids
may be used when acute pancreatitis begins to resolve. Oral feedings low in fat
and protein are initiated gradually. Caf-feine and alcohol are eliminated from
the diet. If the episode of pancreatitis occurred during treatment with
thiazide diuretics, corticosteroids, or oral contraceptives, these medications
are dis-continued. Follow-up of the patient may include ultrasound, x-ray
studies, or ERCP to determine whether the pancreatitis is resolv-ing and to assess
for abscesses and pseudocysts. ERCP may also be used to identify the cause of
acute pancreatitis if it is in ques-tion and for endoscopic sphincterotomy and
removal of gall-stones from the common bile duct.
Related Topics