Chapter: Ophthalmology: Uveal Tract (Vascular pigmented layer)
Acute Iritis and Iridocyclitis
Acute Iritis and Iridocyclitis
Epidemiology:
Iritisis the most frequent form of uveitis. It usually occurs
incombination with cyclitis. About three-quarters of all iridocyclitis cases have an acute clinical course.
Etiology:
Iridocyclitis is frequently attributable toimmunologic causessuchas allergic or
hyperergic reaction to bacterial toxins. In some rheumatic dis-orders it is
known to be frequently associated with the expression of specific human
leukocyte antigens (HLA) such as HLA-B27. Iridocyclitis can also be a symptom of systemic disease such as
ankylosing spondylitis, Reiter’s syn-drome, sarcoidosis, etc. (Table 8.1). Infections are less frequent and occur sec-ondary to penetrating
trauma or sepsis (bacteria, viruses, mycosis, or para-sites). Phacogenic inflammation, possibly with
glaucoma, can result when the lens becomes involved.
Symptoms:
Patients report dull pain in the eye or
forehead accompanied byimpaired vision, photophobia, and excessive tearing
(epiphora).
In contrast to choroiditis, acute iritis or
iridocyclitis is painful because of the involvement of the ciliary nerves.
Diagnostic considerations:
Typical signs include:
❖Ciliary injection: The episcleral and perilimbal vessels may appear blueand red.
❖Combined injection: The conjunctiva is also affected.
The iris is hyperemic (the iris vessels will be visible in a
light-colored iris).
The structure appears diffuse and reactive miosis is present.
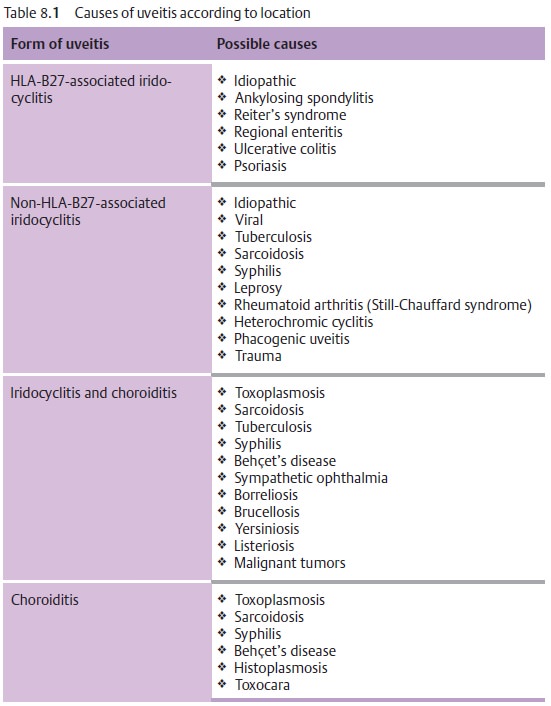
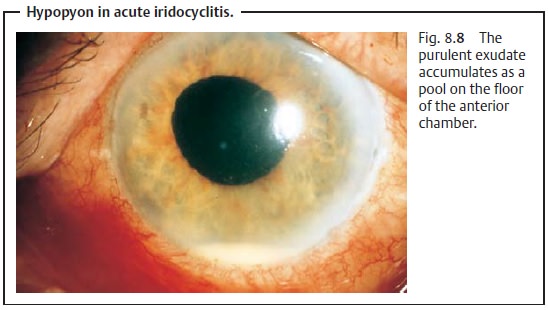
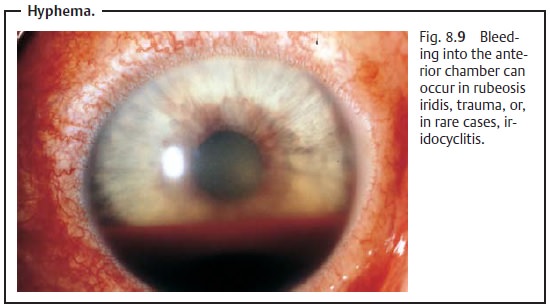
Vision is impaired because of cellular infiltration of the anterior chamber and protein or fibrin accumulation (visible as a Tyndall effect). The precipi-tates accumulate on the posterior surface of the cornea in a triangular con-figuration known as Arlt’s triangle. Exudate accumulation on the floor of the anterior chamber is referred to as hypopyon (Fig. 8.8). Viral infections may be accompanied by bleeding into the anterior chamber (hyphema; Fig. 8.9). Corneal edema can also develop in rare cases.
Corneal edemas and Tyndall effects
(accumulations of protein in the anterior chamber) can be diagnosed when the eye
is illuminated with a lateral beam of light from a focused light or slit lamp.
Differential diagnosis:
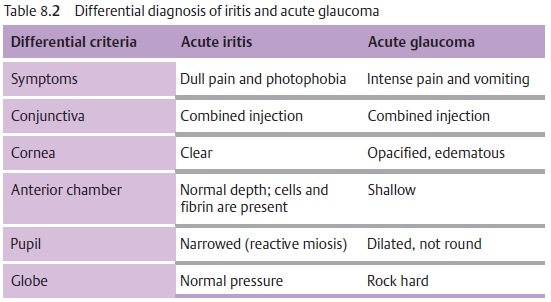
See Table 8.2.
In acute iritis, the depth of the anterior chamber is normal and reactive miosis is present. In contrast, in acute glaucoma the anterior chamber is shallow and the pupil is dilated (Table 8.2).
Complications:
These include:
❖ Secondary open angle glaucoma with an increase in intraocular pressure.
❖ Adhesions between the iris and posterior surface
of the cornea (anterior synechiae).
❖
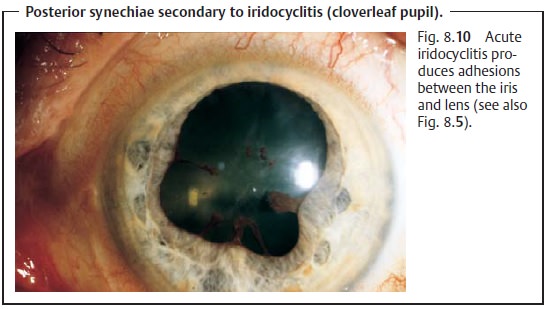
Adhesions between the iris and lens (posterior synechiae; Fig. 8.10).
Treatment:
Topical and, in appropriate cases, systemic antibiotic or antiviraltherapy is indicated for iridocyclitis due to a pathogen (with a corneal ulcer, penetrating trauma, or sepsis).
A conjunctival smear, or a blood culture in
septic cases, is obtained to identify the pathogen. Antibiotic therapy should
begin immediately as microbiological identification of the pathogen is not
always successful.
Therapeutic mydriasis in combination with
steroid therapy is indicated to minimize
the risk of synechiae.
Where no pathogen can be identified, high-dose
topical steroid therapy (prednisolone eyedrops every hour in combination with
subconjunctival injections of soluble dexamethasone) is administered. To
minimize the risk of posterior synechiae,
the pupil must be maximally dilated (atropine,scopolamine, cyclopentolate,
and possibly epinephrine and epinephrine eye-drops).
The mydriatic effect of dilating eyedrops may
be reduced in iritis. This may necessitate the use of longer-acting medications
such as atropine, which may have to be applied several times daily.
Occasionally it is possible to break off existing synechiae in this manner, and patches of iris tissue will remain on the
anterior surface of the lens. Second-ary open angle glaucoma is treated by administering beta blockers in
eye-drop form and, in applicable cases, carbonic anhydrase inhibitors
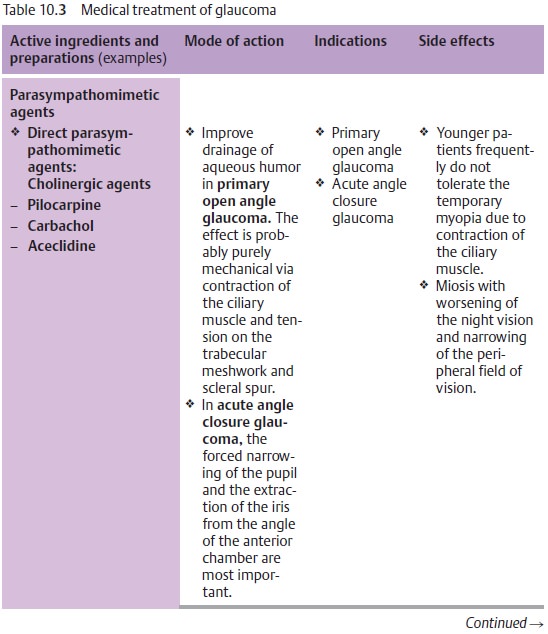
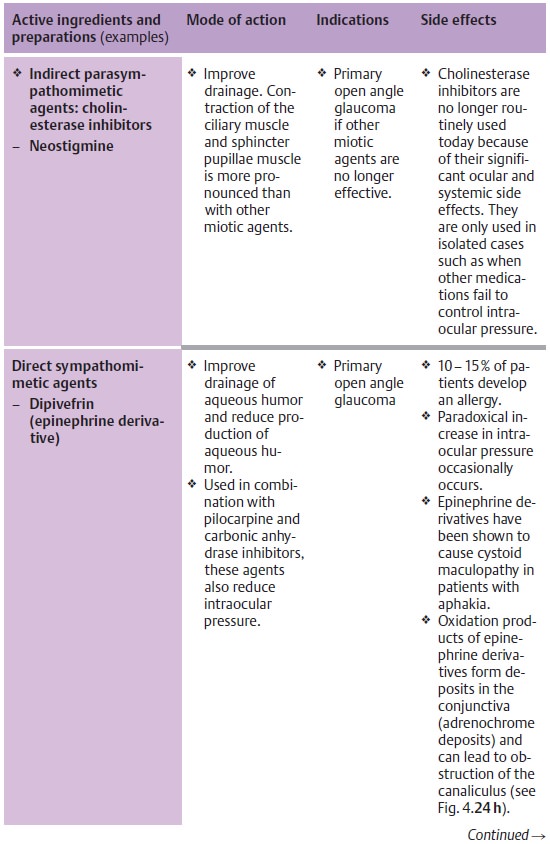
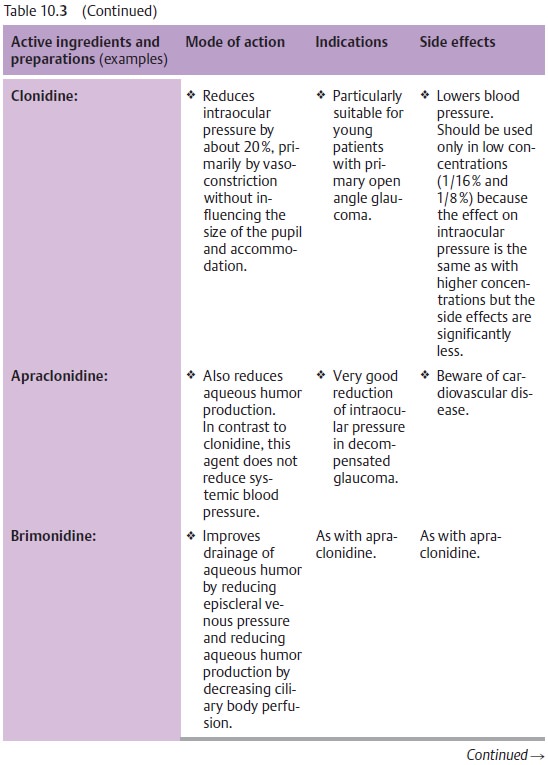
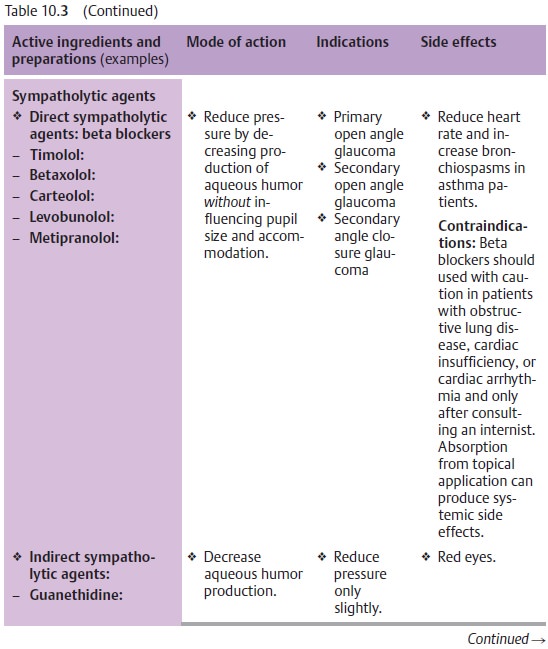
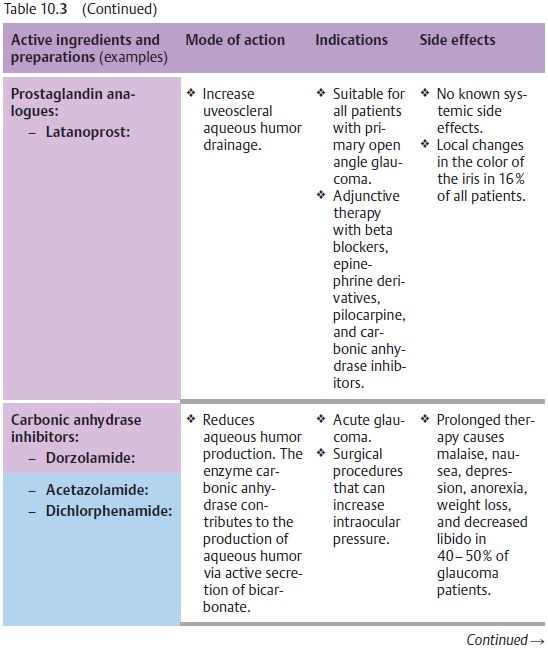
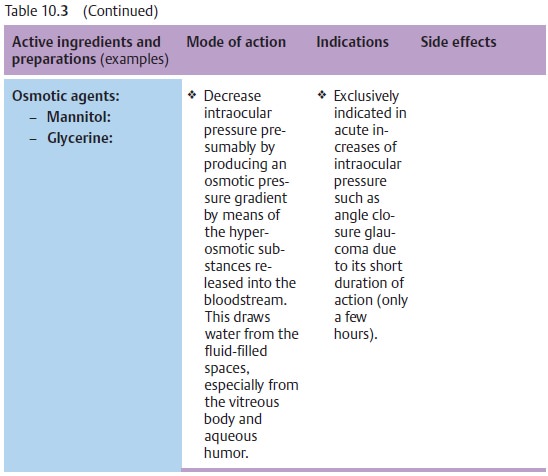
(aceta-zolamide; see Table 10.3).
Prognosis:
Symptoms usually improve within a few days
when proper ther-apy is initiated. The disorder can progress to a chronic
stage.
Related Topics