Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Acne Vulgaris - Secretory Disorders
ACNE VULGARIS
Acne
vulgaris is a common follicular disorder affecting suscepti-ble hair follicles,
most commonly found on the face, neck, and upper trunk. It is characterized by comedones (ie, primary acne lesions),
both closed and open, and by papules, pustules, nodules, and cysts.
Acne is the most commonly encountered skin
condition in adolescents and young adults between ages 12 and 35. Both genders
are affected equally, although onset is slightly earlier for girls. This may be
because girls reach puberty at a younger age than boys. Acne becomes more
marked at puberty and during adolescence because the endocrine glands that
influence the se-cretions of the sebaceous glands are functioning at peak
activity. Acne appears to stem from an interplay of genetic, hormonal, and
bacterial factors. In most cases, there is a family history of acne.
Pathophysiology
During
childhood, the sebaceous glands are small and virtually nonfunctioning. These
glands are under endocrine control, es-pecially by the androgens. During
puberty, androgens stimulate the sebaceous glands, causing them to enlarge and
secrete a nat-ural oil, sebum, which rises to the top of the hair follicle and
flows out onto the skin surface. In adolescents who develop acne, an-drogenic
stimulation produces a heightened response in the se-baceous glands so that
acne occurs when accumulated sebum plugs the pilosebaceous ducts. This
accumulated material forms comedones.
Clinical Manifestations
The
primary lesions of acne are comedones. Closed comedones (ie, whiteheads) are
obstructive lesions formed from impacted lipids or oils and keratin that plug
the dilated follicle. They are small, whitish papules with minute follicular
openings that gen-erally cannot be seen. These closed comedones may evolve into
open comedones, in which the contents of the ducts are in open communication
with the external environment. The color of open comedones (ie, blackheads)
results not from dirt, but from an accumulation of lipid, bacterial, and
epithelial debris.
Although the exact cause is unknown, some closed
comedones may rupture, resulting in an inflammatory reaction caused by leakage of
follicular contents (eg, sebum, keratin, bacteria) into the dermis. This
inflammatory response may result from the action of certain skin bacteria, such
as Propionibacterium
acnes, that live in the hair follicles and break down the triglycerides
of the sebum into free fatty acids and glycerin. The resultant inflam-mation is
seen clinically as erythematous papules, inflammatory pustules, and
inflammatory cysts. Mild papules and cysts drain and heal on their own without
treatment. Deeper papules and cysts may result in scarring of the skin. Acne is
usually graded as mild, moderate, or severe based on the number and type of
lesions (eg, comedones, papules, pustules, cysts).
Assessment and Diagnostic Findings
The diagnosis of acne is based on the history and physical
exam-ination, evidence of lesions characteristic of acne, and age. Acne does
not occur until puberty. The presence of the typical come-dones (ie, whiteheads
and blackheads) along with excessively oily skin is characteristic. Oiliness is
more prominent in the midfacial area; other parts of the face may appear dry.
When there are nu-merous lesions, some of which are open, the person may exude
a distinct sebaceous odor. Women may report a history of flare-ups a few days
before menses. Biopsy of lesions is seldom necessary for a definitive
diagnosis.
Medical Management
The
goals of management are to reduce bacterial colonies, de-crease sebaceous gland
activity, prevent the follicles from becom-ing plugged, reduce inflammation,
combat secondary infection, minimize scarring, and eliminate factors that
predispose the person to acne. The therapeutic regimen depends on the type of
lesion (eg, comedonal, papular, pustular, cystic).
There
is no predictable cure for the disease, but combinations of therapies are
available that can effectively control its activity. Topical treatment may be
all that is needed to treat mild to mod-erate lesions and superficial
inflammatory lesions (ie, papular or pustular).
NUTRITION AND HYGIENE THERAPY
Although
food restrictions have been recommended from time to time in treating acne,
diet is not believed to play a major role in therapy. However, the elimination
of a specific food or food prod-uct associated with a flare-up of acne, such as
chocolate, cola, fried foods, or milk products, should be promoted. Maintenance
of good nutrition equips the immune system for effective action against
bacteria and infection.
For mild cases of acne, washing twice each day with
a cleansing soap may be all that is required. These soaps can remove the
exces-sive skin oil and the comedo in most cases. Providing positive
re-assurance, listening attentively, and being sensitive to the feelings of the
patient with acne are essential contributors to the patient’s psychological
well-being and understanding of the disease and treatment plan.
Over-the-counter acne medications contain sali-cylic acid and benzoyl peroxide,
both of which are very effective at removing the sebaceous follicular plugs.
However, the skin of some people is sensitive to these products, which can
cause irritation or excessive dryness, especially when used with some
prescribed topi-cal medications. The patient should be instructed to
discontinue their use if severe irritation occurs. Oil-free cosmetics and
creams should be chosen. These products are usually designated as useful for
acne-prone skin. The duration of treatment depends on the ex-tent and severity
of the acne. In severe cases, treatment may extend over years.
TOPICAL PHARMACOLOGIC THERAPY
Benzoyl Peroxide.
Benzoyl peroxide preparations are widelyused because they produce a rapid
and sustained reduction of inflammatory lesions. They depress sebum production
and pro-mote breakdown of comedo plugs. They also produce an anti-bacterial
effect by suppressing P. acnes.
Initially, benzoyl peroxide causes redness and scaling, but the skin usually
adjusts quickly to its use. Typically, the patient applies a gel of benzoyl
peroxide once daily. In many instances, this is the only treatment needed.
Benzoyl peroxide, benzoyl erythromycin, and benzoyl sulfur combinations are
available over the counter and by prescription. Vitamin A acid (tretinoin)
applied topically is used to clear the keratin plugs from the pilosebaceous
ducts. Vitamin A acid speeds the cellular turnover, forces out the comedones,
and prevents new comedones.
The
patient should be informed that symptoms may worsen during early weeks of
therapy because inflammation may occur during the process. Erythema and peeling
also frequently result. Improvement may take 8 to 12 weeks. Some patients
cannot tol-erate this therapy. The patient is cautioned against sun exposure
while using this topical medication because it may cause an ex-aggerated
sunburn. Package insert directions should be followed carefully.
Topical Antibiotics.
Topical antibiotic treatment for acne is com-mon.
Topical antibiotics suppress the growth of P. acnes; reduce superficial free
fatty acid levels; decrease comedones, papules, and pustules; and produce no
systemic side effects. Common topical preparations include tetracycline,
clindamycin, and erythromycin.
SYSTEMIC PHARMACOLOGIC THERAPY
Antibiotics.
Oral antibiotics, such as tetracycline,
doxycycline, and minocycline, administered in small doses over a long period
are very effective in treating moderate and severe acne, especially when the
acne is inflammatory and results in pustules, abscesses, and scarring. Therapy
may continue for months to years. The tetracycline family of antibiotics is
contraindicated in children younger than age 12 and in pregnant women. Although
these medications are considered safe for long-term use in most cases,
administration during pregnancy can affect the development of teeth, causing
enamel hypoplasia and permanent discoloration of teeth in infants. Side effects
of tetracyclines include photosensi-tivity, nausea, diarrhea, cutaneous
infection in either gender, and vaginitis in women. In some women,
broad-spectrum antibiotics may suppress normal vaginal bacteria and predispose
the patient to candidiasis, a fungal infection.
Oral Retinoids.
Synthetic vitamin A compounds (ie, retinoids) are
used with dramatic results in patients with nodular cystic acne un-responsive
to conventional therapy. One compound is isotretinoin (Accutane). Isotretinoin
is also used for active inflammatory papu-lar pustular acne that has a tendency
to scar. Isotretinoin reduces sebaceous gland size and inhibits sebum
production. It also causes the epidermis to shed (ie, epidermal desquamation),
thereby un-seating and expelling existing comedones.
The
most common side effect, experienced by almost all pa-tients, is cheilitis (ie, inflammation of the
lips). Dry and chafed skin and mucous membranes are frequent side effects.
Thesechanges are reversible
with the withdrawal of the medication. Most important, isotretinoin, like other
vitamin A metabolites, is teratogenic in humans, meaning that it can have an
adverse ef-fect on a fetus, causing central nervous system and cardiovascular
defects and structural abnormalities of the face. Contraceptive measures for
women of childbearing age are mandatory during treatment and for about 4 to 8
weeks thereafter. To avoid addi-tive toxic effects, patients are cautioned not
to take vitamin A supplements while taking isotretinoin (Odom et al., 2000).
Hormone Therapy.
Estrogen therapy (including progesterone– estrogen
preparations) suppresses sebum production and reduces skin oiliness. It is
usually reserved for young women when the acne begins somewhat later than usual
and tends to flare up at certain times in the menstrual cycle. Estrogen in the
form of estrogen-dominant oral contraceptive compounds may be admin-istered on
a prescribed cyclic regimen. Estrogen is not adminis-tered to male patients
because of undesirable side effects such as enlargement of the breasts and
decrease in body hair.
SURGICAL MANAGEMENT
Surgical
treatment of acne consists of comedo extraction, injections of corticosteroids
into the inflamed lesions, and incision and drainage of large, fluctuant (ie,
moving in palpable waves), nodu-lar cystic lesions. Cryosurgery (ie, freezing
with liquid nitrogen) may be used for nodular and cystic forms of acne.
Patients with deep scars may be treated with deep abrasive therapy (ie,
der-mabrasion), in which the epidermis and some superficial dermis are removed
down to the level of the scars.
Comedones
may be removed with a comedo extractor. The site is first cleaned with alcohol.
The opening of the extractor is then placed over the lesion, and direct
pressure is applied to cause extrusion of the plug through the extractor. Removal
of come-dones leaves erythema, which may take several weeks to subside.
Recurrence of comedones after extraction is common because of the continuing
activity of the pilosebaceous glands.
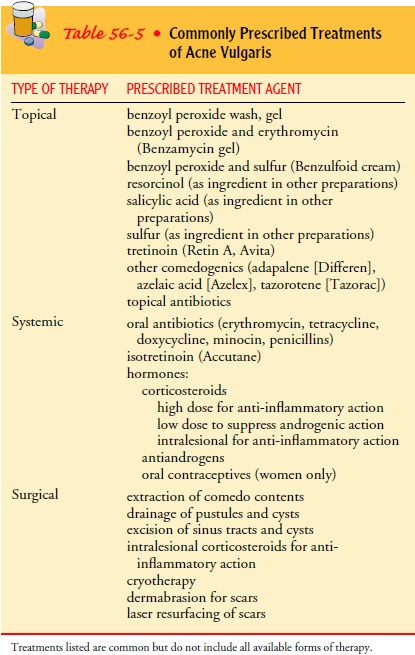
Table
56-5 summarizes the treatment modalities for acne vulgaris.
Nursing Management
Nursing
care of patients with acne consists largely of monitoring and managing
potential complications of skin treatments. Major nursing activities include
patient education, particularly in proper skin care techniques, and managing
potential problems related to the skin disorder or therapy.
PREVENTING SCARRING
Prevention
of scarring is the ultimate goal of therapy. The chance of scarring increases
as the grade of acne increases. Grades III and IV (25 to more than 50
comedones, papules, or pustules) usually require longer-term therapy with
systemic antibiotics or isotretinoin. Patients should be warned that
discontinuing these medications can exacerbate acne, lead to more flare-ups,
and in-crease the chance of deep scarring. Moreover, manipulation of the
comedones, papules, and pustules increases the potential for scarring.
When acne surgery is prescribed to extract deep-seated come-dones or inflamed lesions or to incise and drain cystic lesions, the intervention itself may result in further scarring. Dermabrasion, which levels existing scar tissue, can also increase scar formation. Hyperpigmentation or hypopigmentation also may affect the tissue involved. The patient should be informed of these potential outcomes before choosing surgical intervention for acne.
PREVENTING INFECTION
Female patients receiving long-term antibiotic
therapy with tetra-cycline should be advised to watch for and report signs and
symp-toms of oral or vaginal candidiasis, a yeastlike fungal infection.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
In addition to receiving instruc-tions for taking
prescribed medications, patients are instructed to wash the face and other
affected areas with mild soap and water twice each day to remove surface oils
and prevent obstruction of the oil glands. They are cautioned to avoid
scrubbing the face; acne is not caused by dirt and cannot be washed away.
Mild
abrasive soaps and drying agents are prescribed to elim-inate the oily feeling
that troubles many patients. At the same time, patients are cautioned to avoid
excessive abrasion because it makes acne worse. Excessive abrasion causes
minute scratches on the skin surface and increases possible bacterial
contamina-tion. Soap itself can irritate the skin.
All
forms of friction and trauma are avoided, including prop-ping the hands against
the face, rubbing the face, and wearingtight collars and helmets. Patients are
instructed to avoid manip-ulation of pimples or blackheads. Squeezing merely
worsens the problem, because a portion of the blackhead is pushed down into the
skin, which may cause the follicle to rupture. Because cos-metics, shaving
creams, and lotions can aggravate acne, these sub-stances are best avoided unless
the patient is advised otherwise. There is no evidence that a particular food
can cause or aggravate acne. In general, eating a nutritious diet helps the
body maintain a strong immune system.
Related Topics