Chapter: Medical Physiology: Heart Valves and Heart Sounds; Dynamics of Valvular and Congenital Heart Defects
Abnormal Circulatory Dynamics in Valvular Heart Disease
Abnormal Circulatory Dynamics in Valvular Heart Disease
Dynamics of the Circulation in Aortic Stenosis and Aortic Regurgitation
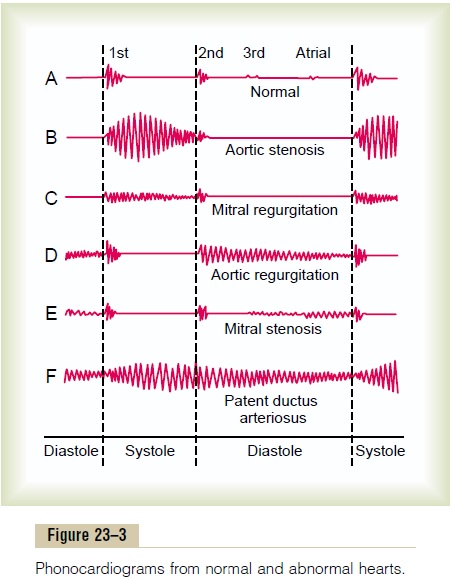
In aortic stenosis, the contracting left ventricle fails to empty adequately, whereas in aortic regurgitation, blood flows backward into the ventricle from the aorta after the ventricle has just pumped the blood into the aorta. Therefore, in either case, the net stroke volumeoutput of the heart is reduced.
Several important compensations take place that can ameliorate the severity of the circulatory defects. Some of these compensations are the following.
Hypertrophy of the Left Ventricle. In both aortic stenosisand aortic regurgitation, the left ventricular muscula-ture hypertrophies because of the increased ventricu-lar workload.
In regurgitation, the left ventricular chamber also enlarges to hold all the regurgitant blood from the aorta. Sometimes the left ventricular muscle mass increases fourfold to fivefold, creating a tremendously large left side of the heart.
When the aortic valve is seriously stenosed, the hypertrophied muscle allows the left ventricle to develop as much as 400 mm Hg intraventricular pres-sure at systolic peak.
In severe aortic regurgitation, sometimes the hyper-trophied muscle allows the left ventricle to pump a stroke volume output as great as 250 milliliters, although as much as three fourths of this blood returns to the ventricle during diastole, and only one fourth flows through the aorta to the body.
Increase in Blood Volume. Another effect that helpscompensate for the diminished net pumping by the left ventricle is increased blood volume. This results from an initial slight decrease in arterial pressure, plus peripheral circulatory reflexes that the decrease in pressure induces. These together diminish renal output of urine, causing the blood volume to increase and the mean arterial pressure to return to normal. Also, red cell mass eventually increases because of a slight degree of tissue hypoxia.
The increase in blood volume tends to increase venous return to the heart. This, in turn, causes the left ventricle to pump with the extra power required to overcome the abnormal pumping dynamics.
Eventual Failure of the Left Ventricle, and Development of Pulmonary Edema
In the early stages of aortic stenosis or aortic regurgi-tation, the intrinsic ability of the left ventricle to adapt to increasing loads prevents significant abnormalities in circulatory function in the person during rest, other than increased work output required of the left ven-tricle. Therefore, considerable degrees of aortic steno-sis or aortic regurgitation often occur before the person knows that he or she has serious heart disease (such as a resting left ventricular systolic pressure as high as 200 mm Hg in aortic stenosis or a left ventric-ular stroke volume output as high as double normal in aortic regurgitation).
Beyond a critical stage in these aortic valve lesions, the left ventricle finally cannot keep up with the work demand. As a consequence, the left ventricle dilates and cardiac output begins to fall; blood simultaneously dams up in the left atrium and in the lungs behind the failing left ventricle. The left atrial pressure rises pro-gressively, and at mean left atrial pressures above 25 to 40 mm Hg, serious edema appears in the lungs.
Dynamics of Mitral Stenosis and Mitral Regurgitation
In mitral stenosis, blood flow from the left atrium into the left ventricle is impeded, and in mitral regurgita-tion, much of the blood that has flowed into the left ventricle during diastole leaks back into the left atrium during systole rather than being pumped into the aorta. Therefore, either of these conditions reduces net movement of blood from the left atrium into the left ventricle.
Pulmonary Edema in Mitral Valvular Disease. The buildupof blood in the left atrium causes progressive increase in left atrial pressure, and this eventually results in development of serious pulmonary edema. Ordinarily, lethal edema does not occur until the mean left atrial pressure rises above 25 mm Hg and sometimes as high as 40 mm Hg, because the lung lymphatic vasculature enlarges manyfold and can carry fluid away from the lung tissues extremely rapidly.
Enlarged Left Atrium and Atrial Fibrillation. The high leftatrial pressure in mitral valvular disease also causes progressive enlargement of the left atrium, which increases the distance that the cardiac electrical exci-tatory impulse must travel in the atrial wall. This pathway may eventually become so long that it pre-disposes to development of excitatory signal circusmovements. Therefore,in late stages of mitral valvular disease, especially in mitral stenosis, atrial fibrillation usually occurs. This further reduces the pumping effectiveness of the heart and causes further cardiac debility.
Compensation in Early Mitral Valvular Disease. As alsooccurs in aortic valvular disease and in many types of congenital heart disease, the blood volume increases in mitral valvular disease principally because of dimin-ished excretion of water and salt by the kidneys. This increased blood volume increases venous return to the heart, thereby helping to overcome the effect of the cardiac debility.Therefore, after compensation, cardiac output may fall only minimally until the late stages of mitral valvular disease, even though the left atrial pres-sure is rising.
As the left atrial pressure rises, blood begins to dam up in the lungs, eventually all the way back to the pul-monary artery. In addition, incipient edema of the lungs causes pulmonary arteriolar constriction. These two effects together increase systolic pulmonary arte-rial pressure and also right ventricular pressure, some-times to as high as 60 mm Hg, which is more than double normal. This, in turn, causes hypertrophy of the right side of the heart, which partially compensates for its increased workload.
Circulatory Dynamics During Exercise in Patients with Valvular Lesions
During exercise, large quantities of venous blood are returned to the heart from the peripheral circulation. Therefore, all the dynamic abnormalities that occur in the different types of valvular heart disease become tremendously exacerbated. Even in mild valvular heart disease, in which the symptoms may be unrec-ognizable at rest, severe symptoms often develop during heavy exercise. For instance, in patients with aortic valvular lesions, exercise can cause acute left ventricular failure followed by acute pulmonaryedema. Also, in patients with mitral disease, exercisecan cause so much damming of blood in the lungs that serious or even lethal pulmonary edema may ensue in as little as 10 minutes.
Even in mild to moderate cases of valvular disease, the patient’s cardiac reserve diminishes in proportion to the severity of the valvular dysfunction. That is, the cardiac output does not increase as much as it should during exercise. Therefore, the muscles of the body fatigue rapidly because of too little increase in muscle blood flow.
Related Topics